 Discussion
Discussion
Myeloma overview
Last updated Dec. 20, 2024, by Marisa Wexler, MS

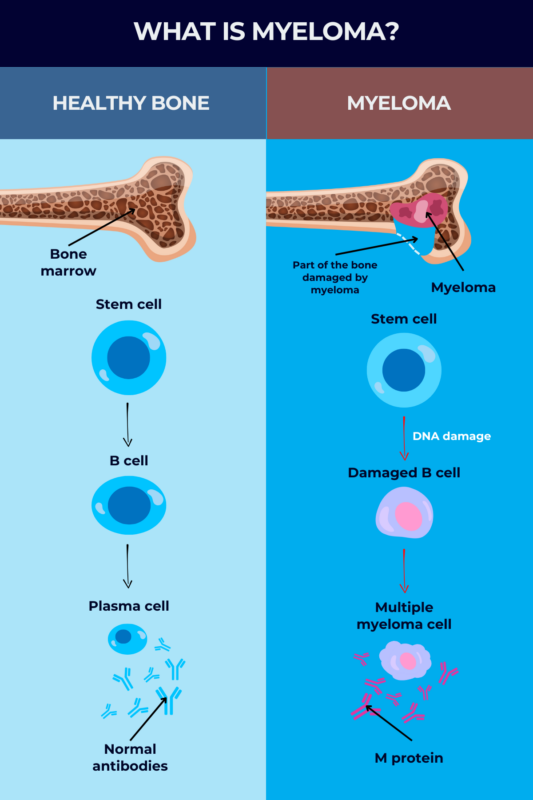
Myeloma is a rare blood cancer that begins in plasma cells, a type of white blood cell responsible for producing antibodies that help fight off infections and other threats.
When plasma cells become cancerous, they grow out of control in the bone marrow, the spongy tissue inside some bones where blood cells are generated. Called myeloma cells, these cancerous cells also produce large amounts of an abnormal antibody, called M protein, which causes a number of complications throughout the body.
Because most myeloma patients have masses of cancer cells in more than one bone marrow location, the disease is often called multiple myeloma. The terms “myeloma” and “multiple myeloma” are often used interchangeably.
Multiple myeloma affects about 7 out of every 100,000 people each year, accounting for about 1.8% of all new cancer diagnoses in the U.S. each year and around 10% of all blood cancers combined. It’s estimated that about 100,000 people in the U.S. have myeloma.
Myeloma can in some cases be a terminal cancer, but with modern medical care, many people with myeloma will live for several years after getting diagnosed.
Causes and risk factors
The causes of myeloma are not fully understood, but like other cancers, the disease is thought to develop due to mutations in the DNA. These mutations may deactivate cellular machinery that normally acts to prevent excessive cell growth, or they may activate signaling that drives cell growth. Whatever the case, the end result is that cells start to grow out of control and ultimately become cancerous.
In the case of myeloma, these mutations occur in plasma cells, which are mature immune B-cells that produce antibodies against a specific target, or antigen. The fact that myeloma is a cancer of the plasma cells differentiates myeloma from leukemia and lymphoma, which are blood cancers that affect other types of white blood cells.
Plasma cell disorders
A few plasma cell disorders, in which the body makes too many plasma cells, may eventually progress to multiple myeloma, and may be seen as risk factors for the disease. Patients with these conditions will have higher-than-normal levels of plasma cells, and some may also have elevated levels of M protein, but those levels are not yet sufficient for a diagnosis of multiple myeloma. Some of these disorders include:
- Monoclonal gammopathy of undetermined significance, or MGUS, a precancerous condition where people have low levels of myeloma cells or M protein. Each year, one out of 100 people with MGUS develop myeloma.
- Smoldering myeloma, another precancerous condition for multiple myeloma where about 10%-60% of cells in the bone marrow are myeloma cells. About 10% of patients with smoldering myeloma will develop active myeloma each year.
- Plasmacytoma, a very rare type of blood cancer where patients have a single mass of myeloma cells in the bone or bone marrow (solitary plasmacytoma) or in soft tissues (extramedullary plasmacytoma). Up to 70% of these patients will go on to develop multiple myeloma after 10 years.
It is now well-established that, for a patient to develop myeloma, they must first pass through the precursor stages of MGUS and smoldering myeloma. While neither of those conditions causes overt symptoms, patients are closely monitored for many years to detect active myeloma as soon as it develops, which can lead to better outcomes.
Other risk factors
In addition to the presence of plasma cell disorders, other risk factors for myeloma include:
- being male
- being Black
- being older than 60
- having history of exposure to radiation, wood dust, fuel oil products, or certain chemicals like insecticides and pesticides
- being obese.
Multiple myeloma is not thought to be a hereditary disease, which means that the mutations that cause it are usually not passed down through families.
Types of myeloma
There are different types of myeloma, depending on the specific abnormal antibodies, or M proteins, produced by the cancerous plasma cells.
Antibodies, also known as immunoglobulins (Ig), consist of two key components: heavy chains and light chains. The type of myeloma a person has depends on the type of heavy and light chains produced by their myeloma cells.
There are five types of these heavy chains: IgG, IgA, IgD, IgE, and IgM, and most people with myeloma will have one of these types present. IgG myeloma is the most common, followed by IgA myeloma. IgM, IgD, and IgE myelomas are rare, occurring in a small percentage of cases.
The two types of light chains are kappa and lambda. Myeloma patients can produce any combination of these heavy and light chains, although IgG kappa is the most common type. In about 15% of patients, myeloma cells produce only a light chain protein and no heavy chain. This is an aggressive form of the disease known as light-chain multiple myeloma.
Symptoms
When myeloma first develops, it often does not cause any obvious early signs and is only detectable through medical testing. However, as the abnormal plasma cells accumulate and spread, and the amount of M protein increases in the bloodstream, patients begin to experience myeloma symptoms, which can include:
- fatigue, and mental fogginess or confusion
- bone pain
- frequent infections
- nausea, constipation, and/or loss of appetite
- unintended weight loss.
Myeloma affects everyone differently, and symptoms can vary from person to person. Other signs and symptoms of myeloma may include:
- high calcium levels (hypercalcemia), which can lead to symptoms such as excessive thirst and needing to urinate often
- weakened bones and a higher risk of broken bones
- low blood count, which can contribute to symptoms like fatigue, weakness, and easy bleeding
- abnormally thick blood (hyperviscosity), which can lead to symptoms such as dizziness and confusion
- nerve damage, which can cause pain, numbness, tingling sensations, and weakness
- kidney problems.
Diagnosis
Diagnosing multiple myeloma begins with a consultation where a doctor will evaluate a patient’s health and family history, and look for telltale signs of the cancer, including bleeding, signs of infection, or areas of bone tenderness.
If multiple myeloma is suspected, a person will be referred to a hematologist, or a physician who specializes in diseases affecting the blood, for further testing and imaging scans.
Medical tests that may be used to diagnose myeloma include:
- blood tests and urine tests, which can be used to detect M protein and other markers of disease
- bone marrow biopsy, which can be used to look for abnormal growth of plasma cells in the bone marrow
- imaging tests, including X-rays and MRI or CT scans, which can help detect areas where myeloma cells are growing and causing bone damage
Traditionally, a myeloma diagnosis can be confirmed when a plasma cell tumor is observed through biopsy or plasma cells make up 10% of the cells in the bone marrow, and patients have at least one of the following:
- low levels of red blood cells
- high blood calcium levels
- bone disease, namely signs of bone damage caused by myeloma cells
- kidney impairment
- increase in one type of light chain in the blood so that it becomes 100 times more common than the other
- at least 60% of plasma cells in the bone marrow.
Multiple myeloma stages
In addition to detecting myeloma, diagnostic tests can be used to establish the stages of myeloma, which provide information about how aggressive the cancer is and how much it has spread in the body. Staging helps doctors to predict how myeloma will progress and decide on an optimal treatment plan.
The Revised International Staging System (R-ISS) is most commonly used to stage myeloma. On the R-ISS, myeloma is classified as one of three stages, depending on the specific genetic abnormalities in the cancer cells, as well as the amount of certain proteins in the blood:
- beta-2-microglobulin
- albumin
- lactate dehydrogenase (LDH).
In stage 1, which is the mildest stage, patients meet all the following criteria:
- less than 3.5 milligrams per litre (mg/L) of beta 2 microglobulin
- 3.5 grams per deciliter (g/dL) or more of albumin
- normal LDH levels
- no high-risk genetic abnormalities in their cancer cells.
In stage 3, the most severe stage, patients have:
- beta 2 microglobulin levels equal to or above 5.5 mg/L, and either
- high LDH levels or
- genetic changes considered high risk.
Stage 2 is used to classify all myelomas that do not meet the criteria for stage 1 or 3. This will include, for example, someone who meets all but one criteria for stage 1, or a person with high-risk genetic changes or elevated LDH levels whose beta 2 microglobulin levels are below 5.5 mg/L.
Stage 3 is the most advanced myeloma, and there is no stage 4.
Treatment
People with the precursor forms of myeloma, MGUS and smoldering myeloma, which is also known as asymptomatic myeloma, usually don’t require immediate treatment, especially if their condition isn’t causing any issues. However, when symptoms occur in active myeloma, treatment becomes necessary to manage the disease.
Many treatment options for myeloma are available, including:
- chemotherapy, which uses drugs that kill rapidly-growing cells and can help destroy myeloma cells
- targeted therapies, such as proteasome inhibitors and immunomodulatory agents, which kill myeloma cells by blocking specific molecular pathways that the cells use to grow and survive
- immunotherapies, such as certain monoclonal antibodies and CAR T-cells, which activate the body’s immune system to attack and destroy cancer cells
- stem cell transplant, which aims to reset the production of new blood cells in the body
- corticosteroids, which are immune-suppressing drugs often given to help other drugs fight the cancer and ease their side effects.
In addition, people with myeloma often benefit from supportive care measures, also known as palliative care, to help deal with disease symptoms and the side effects of treatment. These may include:
- pain management medications
- surgery to help prevent or treat bone fractures
- radiation therapy to manage bone damage caused by myeloma
- blood transfusions and other medications to normalize blood cell counts
- plasmapheresis to remove the excess M protein when the blood becomes too viscous
- dialysis if a person develops kidney failure.
Each type of myeloma treatment has its own unique profile in terms of potential risks and benefits. Patients and their care team should discuss these in detail to develop a treatment plan tailored to the patient, taking into account individual disease characteristics and preferences.
Various clinical studies are ongoing with the hopes of developing new and potentially more effective myeloma treatments.
Myeloma prognosis and survival rate
With modern medical care, the five-year survival rate for multiple myeloma is about 60%. In other words, approximately 6 out of every 10 people with myeloma will be alive five years after the cancer is diagnosed.
However, myeloma life expectancy and prognosis can vary substantially depending on many factors, including the person’s age, ability to tolerate certain treatments, and the presence of other underlying health problems. One of the most informative factors for predicting survival outcomes is the R-ISS disease stage:
- in R-ISS stage 1, the five-year survival rate is about 82%
- in R-ISS stage 2, the five-year survival rate is approximately 62%
- in R-ISS stage 3, the five-year survival rate is about 40%.
Each multiple myeloma diagnosis is unique and while survival statistics can offer some insight, they do not fully capture the complexity and variability of each person’s experience with the disease.
Living with myeloma
For certain individuals with multiple myeloma, treatment can effectively eliminate or control the disease, but the cancer may persist or return in some cases despite treatment.
Living with myeloma can be challenging and distressing. The journey after a diagnosis involves embracing familiar aspects of life while adapting to new circumstances and making informed decisions for the future.
Prioritizing self-care plays a crucial role in maintaining overall health and improving the quality of life for those with myeloma. Some self-care practices that can significantly contribute to one’s well-being include:
- adopting a well-balanced diet to help support the body
- avoiding smoking, which can weaken the immune system and may also exacerbate symptoms or interfere with treatment effectiveness
- ensuring adequate rest
- practicing good hygiene, including regular hand washing, to minimize the risk of infections
- collaborating with healthcare professionals to establish safe and appropriate exercise routines to maintain physical strength and improve overall well-being
- developing healthy outlets for emotional support and maintaining mental health, which can be beneficial in navigating the emotional challenges that often accompany a myeloma diagnosis.
No one has to go through a myeloma diagnosis alone. Support groups exist that can help those affected by myeloma:
- The International Myeloma Foundation offers support groups to empower patients and care partners with information, insight, and education.
- The Multiple Myeloma Research Foundation offers support groups and other resources to help people with myeloma navigate life with the disease.
- The Cancer Survivors Network, part of the American Cancer Society, offers a support community for cancer patients, survivors, caregivers, and families.
Rare Cancer News can also be a resource for those with myeloma, their caregivers, and their loved ones, providing the latest in research and treatment advances as well as educational resources.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Why false stories about caregiving can be harmful
- New targeted therapy for childhood brain cancer nears European approval
- New trial data show alnodesertib may slow ovarian cancer progression
- IMF launches Myeloma Action Month to raise global awareness this March
- Annamycin shows encouraging early results in Phase 2/3 AML clinical trial
Related articles
-
 Discussion
Discussion
-





