Treatment for pancreatic cancer
Last updated March 28, 2025, by Lindsey Shapiro, PhD

Treatment for pancreatic cancer, a rare cancer that arises from cells in the pancreas, may involve a variety of different approaches, depending on factors such as the stage of disease and a person’s health status.
Due to the aggressive nature of the disease, pancreatic cancer survival rates are relatively low. An early diagnosis, when the cancer can still be treated with potentially curative surgery, is critical to improve a person’s pancreatic cancer prognosis. When surgery is not an option, chemotherapy, radiation, and other supportive care measures may help control the cancer and keep patients comfortable for as long as possible.
As every person is different, each pancreatic cancer patient will experience different symptoms and side effects that require personalized care. Patients should work closely with their doctors to understand their treatment options and how their symptoms can best be managed in their case.
How is pancreatic cancer treated?
There are a number of different treatment options for pancreatic cancer, including surgery, chemotherapy, and radiotherapy, as well as medications and other supportive therapies that help manage symptoms and treatment side effects. The treatment that’s used for any given patient will depend on factors that include:
- the type of pancreatic cancer
- where the tumor is located within the pancreas
- how advanced the disease is, including the tumor’s size and if it has spread
- the person’s general health.
Treating pancreatic cancer usually requires a multidisciplinary team that includes experts such as an oncologist, a surgeon, a gastroenterologist, a radiologist, a dietitian, and a specialized cancer nurse, among others. This healthcare team works together with the patient to create a tailored treatment plan that will work best in that individual case.
A person may receive one or multiple treatment types at various pancreatic cancer stages. They’ll also be monitored regularly to determine how they’re responding to pancreatic cancer treatment and whether the plan needs to change.
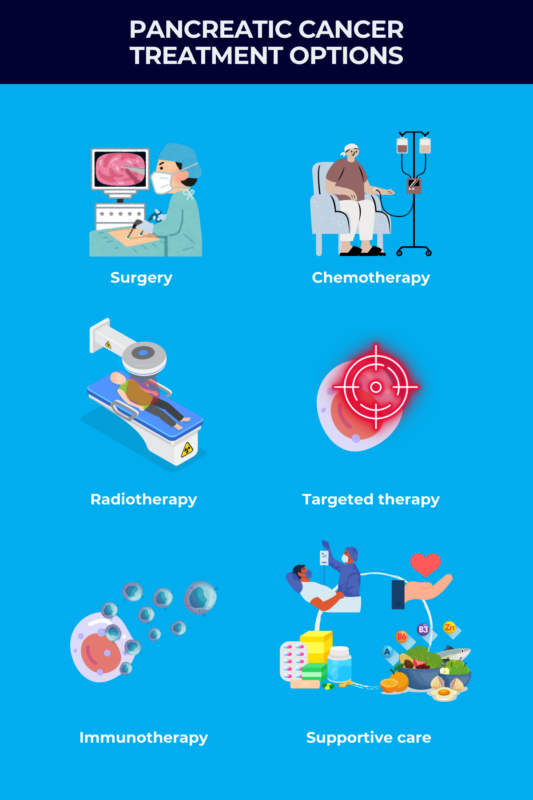
Surgery
The preferred option for treating pancreatic cancer is surgery to completely remove, or resect, the tumor. This is the only treatment that can potentially cure patients from cancer.
However, this approach is only feasible in the small number of people whose cancer is diagnosed early on — usually in stage 1 and stage 2 pancreatic cancer — when the tumor is limited to the pancreas and has not spread to nearby lymph nodes or other organs. As partially removing the cancer is not associated with improved survival, a surgeon will only consider the procedure if it’s believed the cancer can be completely removed.
While surgery is the only realistic way that pancreatic cancer can be cured, it is not a guarantee that it will do so. Even when all visible cancer is removed during surgery, there could still be some cancer cells that have spread to other regions in the body, which may form new tumors over time.
Surgery for pancreatic cancer is generally a very complex procedure, so this approach is only an option if a person’s health is considered good enough for them to tolerate and recover effectively from the operation. Those with serious health issues, such as severe heart or lung disease, may not be able to have surgery.
Surgeries to resect pancreatic cancer
The pancreas is shaped like a flat pear, with a wide end called the head, middle portions called the neck and body, and a thin end known as the tail. There are a few different types of surgery that might be used to remove pancreatic cancer, the choice of which depends on the location of the tumor and how much of the pancreas is affected. They are a:
- pancreatoduodenectomy, or Whipple procedure
- distal pancreatectomy
- total pancreatectomy.
A Whipple procedure is the most common type of pancreatic cancer surgery. It’s used when cancer affects the head of the pancreas.
During a Whipple surgery for pancreatic cancer, a surgeon will remove the head of the pancreas, as well as several surrounding tissues, including the lower end of the stomach, the first part of the small intestine (duodenum), the gallbladder, part of the bile ducts, and some nearby lymph nodes. Then, the remaining parts of the stomach and bile ducts, which carry the digestive fluid bile from the liver to the small intestine, are reconnected to the small intestine, and the rest of the pancreas is rejoined to the small intestine or the stomach.
A modified Whipple procedure called a pylorus-preserving pancreatoduodenectomy may also be considered when the head of the pancreas is affected. This procedure preserves the stomach and is believed to help with digestion after the surgery, but there’s no evidence that one is better than the other for treating pancreatic cancer.
If other parts of the pancreas are affected, a distal pancreatectomy may be performed. This removes the body and tail of the pancreas, as well as the nearby spleen.
A surgery to remove the entire pancreas — total pancreatectomy — may be performed if the tumor is large or if there is more than one tumor. The surgeon will also remove the duodenum, the gallbladder and part of the bile duct, the spleen, and possibly part of the stomach. The stomach and bile ducts are then joined to the small intestine.
In some cases, the tumor is limited to the pancreas, but may be too close to major blood vessels. These patients may first need to undergo chemotherapy and/or radiation therapy to shrink the tumor enough to make surgery possible.
Palliative surgery
When potentially curative surgery is not an option, there are other surgeries that may be performed to ease certain pancreatic cancer symptoms. These are known as palliative surgeries.
For some people, pancreatic cancer causes blockages in the duodenum or the bile ducts. These blockages can cause symptoms such as jaundice, that is, a yellowing of the eyes and skin, nausea, vomiting, and several other problems.
Surgeons can perform surgical procedures called bypass surgeries, where they make new connections between organs to get around these blockages. A less invasive and more common option is a biliary stent placement, where a tube-shaped device called a stent is placed in the bile duct to keep it open, even if the cancer presses on it.
Recovering from surgery
After surgery, a patient will likely need to stay in the hospital for one to two weeks, or sometimes longer if complications arise. These surgeries are major procedures, so even after going home, a person can expect recovery will take at least a few months, or possibly longer.
In some cases, patients will undergo chemotherapy after they’ve recovered from surgery to prevent their cancer from coming back.
Surgery Risks
Pancreatic cancer surgery to remove pancreatic tumors is a major and complex procedure that comes with a relatively high risk of possibly life-threatening complications. These may include:
- leaking from the connections between organs the surgeon has joined
- bleeding
- infections
- blood clots
- reactions to the anesthesia.
The pancreas is involved in making enzymes important for digestion and hormones for sugar control. Thus, removing a part or the whole pancreas during pancreatic cancer surgery can lead to:
- digestive problems that require pancreatic enzyme replacement therapy (PERT)
- weight loss
- diabetes.
These side effects are a possibility with a Whipple or a distal pancreatectomy, but are certain with a total pancreatectomy.
Chemotherapy
Chemotherapy refers to a large class of medications that work in different ways to stop the growth of cancer cells. People with pancreatic cancer might have chemotherapy:
- to ease symptoms and control cancer for as long as possible when surgery is not an option
- to shrink a tumor before surgery
- to prevent cancer from returning after surgery.
Chemotherapy for pancreatic cancer can be used at any stage, but it may be a key component of care for people with stage 3 or stage 4 pancreatic cancer, for whom surgery is usually not possible.
There are several approved pancreatic cancer chemotherapy drugs. Some common ones include:
- gemcitabine
- 5-fluorouracil
- capecitabine
- Abraxane (albumin-bound paclitaxel)
- irinotecan
- cisplatin
- oxaliplatin.
Patients may receive one or a combination of chemotherapy agents, depending on their specific situation and their health status. Some medications are infused into the bloodstream at a healthcare clinic and others are taken orally.
Chemotherapy is usually given in cycles, with specific treatment days and periods of rest in between, but the exact schedule will depend on the chemotherapy agents that are being used.
Chemotherapy side effects
Chemotherapy drugs are very powerful. In addition to killing cancer cells, they can affect other healthy cells in the body, leading to a wide range of side effects. Each specific medication will have its own side effect profile.
Common chemotherapy side effects include:
- feeling sick or nauseated
- reduced appetite and weight loss
- increased risk of infection
- fatigue, tiredness, or weakness
- bruising, bleeding gums, or nose bleeds
- diarrhea or constipation
- hair loss.
Patients should let their doctors know about any chemotherapy-induced side effects they might be experiencing, as there are many supportive care measures that can help relieve them. If a chemotherapy regimen is not well tolerated, there may also be other options.
Radiation therapy
Radiation therapy uses high-energy radiation, usually from X-rays, to kill cancer cells or stop them from growing and spreading. In people with pancreatic cancer, radiation therapy may be given:
- before surgery, to lower the risk that cancer cells will be left behind
- after surgery, to kill any remaining cancer cells and prevent cancer from returning
- to prevent tumor growth and ease symptoms such as pain when surgery is not possible.
Radiation therapy for pancreatic cancer is commonly given in combination with chemotherapy. In most cases, patients receive external beam radiation therapy, where a machine outside the body directs radiation through the skin to the area where the tumor is located.
Radiation generally works by damaging the DNA of cancer cells. But because it can also cause damage to healthy cells, radiation beams are directed to the cancer as precisely as possible.
There are several specialized methods to reduce the amount of radiation that’s delivered to healthy tissues. A doctor will help patients understand which type is best in their particular case and determine if patients should receive single radiation sessions or a series of daily treatments over a given period.
Radiation therapy itself is not painful. While the side effects of radiation therapy can vary depending on the type administered, some of the most common ones include:
- nausea
- loss of appetite
- diarrhea
- fatigue and weakness
- darkening of the skin or hair loss where treatment occurred.
Targeted therapy
Cancer cells develop DNA mutations that give them a survival advantage, helping them survive and grow regardless of the body’s regulatory mechanisms. These mutations are not found in healthy cells, so targeting the resulting proteins or other cellular pathways that the mutated cells hijack to survive is another approach to treating cancer.
In general, therapies that are tailored to a tumor’s genetic makeup are called targeted therapies. Unlike chemotherapy, which indiscriminately kills both cancer and healthy cells, these therapies focus on unique aspects of cancer cells. This minimizes damage to healthy cells, often resulting in fewer side effects compared with chemotherapy.
There are several targeted therapies approved to treat pancreatic cancer in the U.S., each indicated for cancers with specific genetic mutations. They are:
- Tafinlar (dabrafenib) plus Mekinist (trametinib), for BRAF mutations
- Vitrakvi (larotrectinib) and Rozlytrek (entrectinib), for NTRK mutations
- Retevmo (selpercatinib), for RET mutations
- Krazati (adagrasib), for KRAS mutations
- Tarceva (erlotinib), for EGFR mutations
- Lynparza (olaparib), for BRCA1 or BRCA2 mutations
These therapies are taken as pills and are generally intended for people with unresectable pancreatic cancer, or cancer that cannot be removed with surgery. To be eligible, a person will need to undergo testing to see if their cancer cells have the genetic profile targeted by that treatment.
For people with pancreatic neuroendocrine tumors, or PNETs, a type of pancreatic cancer that starts in hormone-producing cells in the pancreas, there are some targeted therapies that may be used when surgery is not an option. They are:
- sunitinib (sold as Sutent, with generics also available)
- Cabometyx (cabozantinib)
- everolimus (sold as Afinitor and others)
- Welireg (belzutifan), for PNETs associated with a hereditary condition called von Hippel-Lindau.
People with PNETs whose tumor produces hormones and causes hormone-related symptoms may also be treated with a class of medications called somatostatin analogs, or more simply hormone therapy. These medications can stop the tumors from releasing hormones and ease certain symptoms. They may also sometimes slow tumor growth, but are not a cure for pancreatic cancer.
Immunotherapy
Immunotherapy is a class of medications designed to stimulate a person’s own immune system to target and kill cancer cells more effectively.
Available immunotherapies for people with pancreatic cancer belong to the class of immune checkpoint inhibitors, which work by blocking proteins used by cancer cells to avoid being detected by the immune system. These include Keytruda (pembrolizumab) and Jemperli (dostarlimab-gxly), which can be used to treat pancreatic cancers with certain genetic characteristics. These treatments are considered when surgery is not an option or when other treatments have not worked.
Immunotherapy for pancreatic cancer may work when other treatments haven’t. However, because it works by removing the brakes from the immune system, it can lead to serious and possible life-threatening immune reactions that require close monitoring.
Supportive therapies
Both pancreatic cancer itself and pancreatic cancer treatments can lead to a wide range of health issues and uncomfortable side effects. Supportive care measures are intended to control these symptoms, ease treatment side effects, and help a person cope with the emotional impacts of their cancer diagnosis.
Symptom management
Doctors can have solutions that minimize or eliminate many symptoms and side effects associated with pancreatic cancer and its treatments. It’s important to always let healthcare providers know about any new symptoms, so they can come up with a plan for managing them.
Pain
People with pancreatic cancer often experience pain, especially in the abdomen or back. Healthcare providers may suggest a variety of different approaches for managing pain, depending on its source and severity:
- pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids
- nerve blocks, to block pain signals from the brain
- nondrug treatments, such as massage, acupuncture, meditation, or physical therapy.
Diabetes
People with pancreatic cancer may develop diabetes as a complication of the disease or after surgery to remove the tumor. This is called type 3c diabetes, where the pancreas is no longer able to produce enough insulin and glucagon, the hormones that control blood sugar levels.
A doctor will monitor a patient’s blood sugar and develop a management plan that may involve:
- tablets to increase insulin production
- insulin injections
- dietary changes.
Other interventions
Healthcare providers may also give patients a variety of other treatments to manage symptoms and pancreatic cancer treatment side effects. These include:
- nausea medications
- sleep aids
- laxatives or antidiarrheals for gastrointestinal problems
- anticoagulants to prevent and treat blood clots.
Nutrition
The pancreas is essential for digestion and pancreatic cancer can prevent the body from absorbing enough nutrients from food. Moreover, cancer and its treatments can cause gastrointestinal symptoms such as stomach pain, nausea, bloating, constipation, or diarrhea, which can make eating difficult and cause weight loss.
Maintaining proper nutrition and staying hydrated are critical for supporting health during treatment and reducing the risk of infections. Patients may benefit from working with a nutritionist or dietician to develop a diet rich in easily digestible, high-protein foods that provide them with enough energy.
Some patients, mainly those who undergo surgery to remove part or the whole pancreas, may require PERT, which provides essential pancreatic digestive enzymes. PERT is taken as oral capsules with food, with the dose varying based on how much a person is eating.
Mental health support
Coping with pancreatic cancer can take a significant toll on a person’s well being. A critical part of pancreatic cancer management is making sure that patients have adequate mental health support.
This will look different for every person based on their specific needs, but may include:
- taking medications for depression or anxiety
- talking with a mental health professional
- finding a support group.
Palliative care
Many treatment centers have a dedicated palliative care team focused on making cancer patients comfortable and minimizing the impact of symptoms and side effects on their lives. Essentially, the goal of palliative care is to enable patients who can’t be cured to live as well as possible at any stage of their disease.
In most cases, pancreatic cancer is diagnosed at more advanced stages, when curative surgery is no longer an option. For those with a terminal diagnosis, pancreatic cancer palliative care is a critical part of disease management, making sure patients have the best possible quality of life in the months or years they have left.
As the end of life approaches, families may consider transitioning to hospice care, which focuses on relieving symptoms and maximizing comfort in a person’s final days. This may include medical and physical care in addition to emotional or spiritual support. Hospice care can be provided at home or in dedicated facilities.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Clearnote’s blood test uses AI to spot pancreatic cancer in high-risk groups
- Being a caregiver requires constant, sometimes impossible, calculations
- Immuno-gene therapy for brain cancer tumors now on FDA fast track
- FDA approves Keytruda for hard-to-treat gynecological cancers
- FDA reviewing new iberdomide combo for hard-to-treat multiple myeloma