Pancreatic cancer overview
Last updated Dec. 13, 2024, by Lindsey Shapiro, PhD

Pancreatic cancer is a rare form of cancer that begins in the pancreas, an essential organ involved in digestion and blood sugar control, but can spread, or metastasize, to other parts of the body.
The disease can cause symptoms such as abdominal pain, nausea, fatigue, and jaundice, or a yellowing of the skin and eyes. However, diagnosing pancreatic cancer is difficult because most of its symptoms are unspecific and don’t become evident until the disease has already advanced significantly. For the majority of patients, potentially curative surgery is no longer an option by the time the disease is diagnosed, so treatment aims largely to control symptoms and prolong survival.
Pancreatic cancer accounts for about 3% of all cancer cases in the U.S., with an estimated 60,000 people diagnosed each year. While rare, it is the third leading cause of cancer deaths, with approximately 47,000 people dying from pancreatic cancer annually in the U.S.
What is pancreatic cancer?
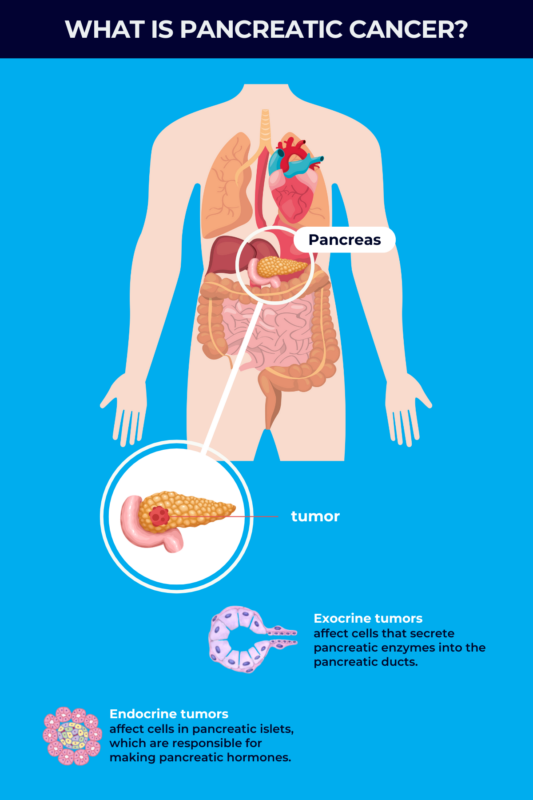
At its core, cancer is a disease in which DNA mutations disrupt normal cellular functions and cause cells to grow uncontrollably, forming tumors that take over and damage healthy tissue. In pancreatic cancer, this process happens to cells in the pancreas.
The pancreas is a digestive organ found in the abdomen behind the lower part of the stomach. It has two main functions: making enzymes that help with food digestion, and producing hormones that are needed to regulate blood sugar levels.
About 15 cm, or six inches, long and pear-shaped, the pancreas has a wide end called the head, middle sections called the neck and body, and a thin end known as the tail. Pancreatic cancer can occur in any part of the organ, but about 60%-70% of cases start in the head.
Types
Pancreatic tumors can be classified as either exocrine or endocrine, depending on the specific cells in the pancreas that are involved.
- Pancreatic exocrine tumors, which account for about 93% of pancreatic tumors, start in the pancreas’ exocrine cells. These cells are responsible for making digestive enzymes.
- Pancreatic endocrine tumors begin in endocrine cells, which are responsible for making pancreatic hormones. Also known as pancreatic neuroendocrine tumors (PNETs) or islet cell tumors, they account for less than 10% of pancreatic tumors.
The vast majority of pancreatic exocrine cancers are adenocarcinomas, which start in the cells lining the ducts that carry digestive enzymes out of the pancreas. There also are many other less common types of exocrine cancers.
While PNETs arise from hormone-producing cells, these tumors often are nonfunctional, meaning they don’t produce any hormones. However, some functional tumors do produce hormones and cause hormone-related symptoms.
In addition to endocrine and exocrine cancers, other rarer types of pancreatic cancer can occur. These are treated differently from the more common types of pancreatic cancer. Among them:
- Pancreatoblastoma, a very rare cancer, is mainly found in children, and starts in the early cells that line the glands in the pancreas.
- Sarcoma of the pancreas is an extremely rare cancer that starts in the connective tissue that holds pancreas cells together.
- Pancreatic lymphoma, a rare form of lymphoma, arises from immune cells in the pancreas.
When a person receives a pancreatic cancer diagnosis, it is important to understand which type of cancer the individual has, as each will have distinct symptoms, management strategies, and prognoses. For example, PNETs often grow slower and have a better prognosis than pancreatic exocrine cancer.
Causes and risk factors
Any person can develop pancreatic cancer, and in most cases, there are no clear pancreatic cancer causes. However, some risk factors may make a person more susceptible. These include genetics and age, as well as certain lifestyle factors or environmental exposures; these latter factors can be modified in many cases to lower an individual’s risk of the disease.
Genetics
About 10% of pancreatic cancer cases are hereditary, meaning the mutation that increased the risk of pancreatic cancer was inherited from a parent. Individuals with one or more first-degree relatives — parents, children, or siblings — with pancreatic cancer may have inherited a mutation that increases their risk of developing the disease.
In addition to a family history of pancreatic cancer, certain mutations or a history of other hereditary conditions may be linked to a greater risk of developing pancreatic cancer. These may include:
- BRCA1 or BRCA2 gene mutations
- PALB2 gene mutations
- Peutz-Jeghers syndrome
- familial atypical multiple mole melanoma
- Lynch syndrome, or hereditary nonpolyposis colorectal cancer
- hereditary pancreatitis, or inflammation of the pancreas
- cystic fibrosis
- familial adenomatous polyposis.
Other genetic conditions can also be specifically associated with an increased risk of developing PNETs, including:
- neurofibromatosis type 1
- multiple endocrine neoplasia type 1
- Von Hippel-Lindau syndrome.
Other risk factors
A number of other factors also are associated with an increased risk of pancreatic cancer. Having these pancreatic cancer risk factors does not mean a person will definitely develop cancer, but it does mean they may be more likely to have it. Still, some of these factors may be modified to reduce a person’s lifetime chances of developing pancreatic cancer.
These factors include:
- smoking or using other forms of tobacco
- heavy alcohol use
- eating red meat
- having type 2 diabetes
- being of an older age
- being overweight or obese
- being exposed to certain chemicals, such as pesticides.
Symptoms
In its earliest stages, when the cancer is still limited to the pancreas, there usually are not any overt signs of pancreatic cancer.
Symptoms become obvious in many cases once the tumor affects other organs of the digestive system. Even then, however, the more advanced signs of pancreatic cancer can still be vague and overlap with those of many other conditions, including certain liver diseases. Many people report intermittent back or stomach pain as early signs of pancreatic cancer.
Other pancreatic cancer symptoms may include:
- jaundice, a yellowing of the skin or whites of the eyes
- dark urine and light-colored stools (poop)
- reduced appetite and weight loss
- fatigue or abnormal physical weakness
- nausea and vomiting
- gas or bloating
- new-onset diabetes or diabetes that’s getting harder to control
- blood clots.
People with PNETs may experience additional symptoms, depending on the type of tumor and the hormones it produces.
In general, the type and frequency of symptoms do not differ by sex. Pancreatic cancer symptoms in men are generally similar to pancreatic cancer symptoms in women.
Diagnosis
To maximize the chances of successful treatment, it is important to catch pancreatic cancer as early as possible. However, because it rarely causes symptoms early on, reaching a pancreatic cancer diagnosis before it has spread to other organs can be challenging.
No universal screening test exists for pancreatic cancer, but people at a high risk of the disease, including those with a family history, should discuss a monitoring plan with their doctors. Monitoring will increase the chances of the disease being diagnosed at an early, more treatable stage.
How do you test for pancreatic cancer?
When a person has symptoms of pancreatic cancer, a doctor will conduct a thorough medical and family history and perform a physical exam. Because the pancreas is deep in the body and difficult to feel in a routine exam, the clinician likely also will order a variety of other diagnostic tests to get more information about what’s going on.
Certain tests may be used to help diagnose pancreatic cancer:
- Imaging tests, including CT and MRI scans, help to visualize the pancreatic tumor and see if the cancer has spread to other organs.
- A biopsy requires a small sample of tissue to be collected and analyzed under a microscope. It helps to establish whether the tumor is cancerous, and to determine what type of pancreatic cancer a person has.
- Blood tests measure markers that pancreatic cancer cells make. These can help support a pancreatic cancer diagnosis, but no blood test can definitively establish a diagnosis on its own.
Different stages
After pancreatic cancer is diagnosed, doctors will determine its stage — meaning how large it is and the extent to which it has spread. Determining the stage is used to establish a person’s pancreatic cancer prognosis, and to decide what treatment would be best for the patient. There are five pancreatic cancer stages — from 0 to 4 — going from most to least treatable, and best to worst prognosis.
Stage 0
At this stage, the tumor is not yet considered cancerous and is still confined to the top layers of the pancreas. The abnormal cells have not invaded deeper tissues nor spread to regions outside the pancreas. However, the cells are at risk of becoming cancerous and spreading to affect normal nearby tissue. This stage is also called carcinoma in situ.
Stage 1
Stage 1 is marked by cancer that’s found only in the pancreas and has not spread elsewhere, including nearby lymph nodes. It can be divided into two substages based on whether the tumor is 2 cm or smaller, when it’s considered stage 1A, or between 2-4 cm, or stage 1B.
This is the most treatable stage, and surgical removal of the tumor is usually possible. Still, there may not be any symptoms of stage 1 pancreatic cancer.
Stage 2
In stage 2 pancreatic cancer, the cancer has started to grow larger and extend its reach. In stage 2A disease, pancreatic cancer is larger than 4 cm across but remains confined to the pancreas. In stage 2B, the cancer may be any size but it has spread to up to three nearby lymph nodes.
Pancreatic cancers in stage 1 or 2 are all considered early cancers and are usually treatable with surgery. About 20% of patients are diagnosed at Stage 1 or 2.
Stage 3
When a person is diagnosed with stage 3 pancreatic cancer, it means the individual has a cancer of any size that’s spread to more regions outside the pancreas. These may include:
- four or more nearby lymph nodes
- nearby major blood vessels, with or without lymph node involvement.
At this stage, the cancer may start to cause symptoms. It also becomes more difficult to treat, and surgery may no longer be possible. About 30% of pancreatic cancers are first diagnosed as stage 3.
Stage 4
At this stage, the cancer can be any size, but it has spread to more distant organs such as the liver, lungs, abdominal cavity, or bones. Stage 4 pancreatic cancer, also called metastatic pancreatic cancer, is when symptoms are more likely to become evident, with about half of all pancreatic cancers being diagnosed at this stage. Still, it is difficult to treat and generally considered incurable.
Treatment
Pancreatic cancer treatment depends on the stage at which the disease is diagnosed and where exactly the tumor is located, as well as on other health conditions the patient may have. Generally, a multidisciplinary healthcare team will determine the best treatment approach for each individual patient. Treatment may involve surgery, chemotherapy, radiotherapy, and other forms of supportive care.
Surgery
Surgery to remove the tumor is the only potentially curative treatment option for pancreatic cancer. However, this procedure is only possible for the approximately 20% of cases that are diagnosed at early stages, when the cancer has not spread to regions outside the pancreas.
The most common type of surgery, called a Whipple or a pancreatoduodenectomy, involves removing the head of the pancreas, as well as other parts of the digestive system that are close to the pancreas. During surgery, the remaining organs are connected to allow food to move through the person’s system.
Other procedures also may be used, which typically depend on the location of the tumor. If the cancer cannot be removed, there are other types of surgery that may be performed to help ease some symptoms.
Chemotherapy and other medications
Chemotherapy refers to a large class of medication types that work to stop the growth of cancer cells. They may be given via the bloodstream (intravenously), or taken orally. In pancreatic cancer, chemotherapy may be used:
- to control symptoms when surgery is not possible
- to help shrink a tumor before surgery to make the procedure more successful
- to stop the cancer from coming back after surgery.
Different chemotherapy drugs may be used to treat exocrine and endocrine tumors. People with PNETs may also be given hormone therapy, which blocks the activity of certain hormones involved in the cancer’s growth.
Radiotherapy
Radiotherapy uses high-energy X-rays to kill cancer cells. It’s often used in combination with chemotherapy. As a pancreatic cancer treatment, radiotherapy may be applied to:
- treat the cancer or control symptoms when surgery is not possible
- shrink a tumor before surgery.
Supportive care
Both pancreatic cancer and cancer treatments can lead to a wide range of symptoms. Supportive care — also called palliative care — aims to manage patient symptoms and improve quality of life, especially in advanced stages where the cancer cannot be cured.
Such support may help with:
- diet and nutrition management
- pain relief
- nausea and sickness control
- fatigue management.
Life expectancy and survival rate
The overall five-year pancreatic cancer survival rate — the percentage of patients who are alive five years after their diagnosis — is about 13%. This has risen from 7% over the last decade, but there’s still an urgent need to improve survival rates in pancreatic cancer.
The stage at which a person is diagnosed has a major impact on the individual’s prognosis. For example, when the cancer is limited only to the pancreas, the five-year survival rate is about 44%. This drops to 16% when the cancer has spread to nearby lymph nodes, and is reduced even further, to about 3%, for metastatic pancreatic cancer.
Diagnosing pancreatic cancer at a stage where it may be treated with surgery can drastically improve outcomes. A recent study found that when pancreatic cancer is diagnosed as early as possible — stage 1A — the five-year survival rates may be higher than 80%.
Survival for PNETs depends on the type of tumor, but this form of pancreatic cancer is generally slower growing and has a better outlook than exocrine cancer. The five-year survival rate for PNETs is higher than 50% overall, rising to 90% when the cancer hasn’t spread.
Still, every person is different and it’s impossible to predict any patient’s exact outcome. Various other factors may influence pancreatic cancer life expectancy, including:
- age
- overall health status
- access to proper treatment and care.
Prevention
Because the cause of pancreatic cancer is usually unknown, there is no sure way to prevent the disease. Still, people can reduce their risk by making certain lifestyle changes, such as:
- maintaining a healthy weight
- avoiding smoking and tobacco products
- limiting alcohol intake
- eating a healthy diet that avoids red meat and highly processed foods
- avoiding exposure to cancer-associated chemicals (carcinogens) at home or at work.
For people who are at an increased risk of pancreatic cancer, including those with a family history or other related conditions, it’s also critical to get regular check-ups and talk with a doctor about a monitoring plan. While this might not necessarily prevent pancreatic cancer, it may help doctors to detect and treat it as early as possible.
Living with pancreatic cancer
Living with pancreatic cancer will affect many aspects of a person’s life and can take a toll on an individual’s mental health. Self-advocacy is one of the most important ways patients can get what they need from their healthcare team and support network. There are some actions people can take to better advocate for themselves:
- Learning more about pancreatic cancer and its treatment options can make patients more informed. Individuals can actively talk with their doctors to gain a better understanding of their particular case and the therapies available to them.
- Communicating with healthcare team members and telling them about any symptoms or pancreatic cancer treatment side effects will help the doctor to better treat the patient. Patients also should take an active role in their cancer care and talk with their doctors about their specific needs.
- Asking for help when necessary is important to let family members, friends, or other caregivers know how they can provide support during pancreatic cancer treatment. Sometimes people want to help but won’t know how.
Resources and support
Building a good support system is key to managing the challenges of pancreatic cancer. That system can include family, friends, mental health professionals, or pancreatic cancer support groups. Doctors’ offices may have a social worker or patient navigator who can help connect patients to helpful support resources.
A number of organizations offer resources and support for people living with pancreatic cancer. Such resources can include financial support, information and educational tools, and support group listings. A few such organizations are:
- the Pancreatic Cancer Action Network
- the National Pancreatic Cancer Foundation
- Project Purple
- Pancreatic Cancer North America.
Rare Cancer News is also a resource for those with pancreatic cancer, their caregivers, and their loved ones. It provides the latest updates in research and treatment advances, as well as educational resources for those who may wish to know more about the condition.
Recent Posts
- Clearnote’s blood test uses AI to spot pancreatic cancer in high-risk groups
- Being a caregiver requires constant, sometimes impossible, calculations
- Immuno-gene therapy for brain cancer tumors now on FDA fast track
- FDA approves Keytruda for hard-to-treat gynecological cancers
- FDA reviewing new iberdomide combo for hard-to-treat multiple myeloma
Related articles