Myeloma treatment
Last updated Oct. 24, 2025, by Marisa Wexler, MS

Multiple myeloma, a type of blood cancer that affects plasma cells in the bone marrow, currently has no known cure, but a number of treatments are available to manage symptoms and slow the progression of the disease.
While myeloma treatment can drive the disease into remission, sometimes for long periods of time, the cancer will often come back after a few months or years, and additional treatments will be needed.
In early stages, treatment may not be necessary for everyone diagnosed with myeloma, especially if the condition is asymptomatic. In such cases, periodic monitoring for any signs of cancer progression is essential. However, once symptoms occur, treatment becomes necessary to manage the disease.
Multiple myeloma cancer treatment often involves a combination of medications, each with their own benefits and risks, to get the best possible results. Understanding the different options available is important to make informed treatment decisions.
Understanding myeloma treatment
Myeloma is a cancer of the plasma cells, a specific type of immune cell that generates antibodies to defend the body against infections and other potential threats.
When plasma cells become cancerous, they grow out of control in the bone marrow, the spongy tissue inside some bones where blood cells are generated. These cancerous cells produce large amounts of an abnormal antibody, called M protein, which causes a number of complications throughout the body.
Because most patients have masses of myeloma cells in more than one bone marrow location, the disease is often called multiple myeloma.
Different strategies are available for myeloma treatment, and the choice of treatment usually depends on factors such as:
- disease stage and extent of organ damage
- overall health of patient
- age of patient
- genetic features of cancer cells
- patient’s specific wishes and desires.
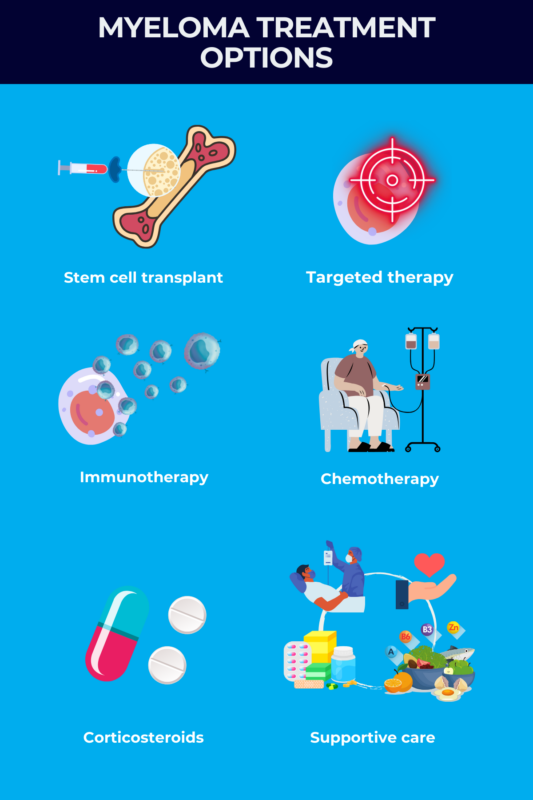
Treatments for myeloma itself generally seek to bring the cancer into remission, meaning that myeloma cells have been mostly eliminated, and the patient is no longer experiencing major complications from myeloma. The most common approaches for treating myeloma, some of which are also used in other types of blood cancer treatment, include:
- stem cell transplant
- targeted therapies, such as proteasome inhibitors and immunomodulatory agents
- immunotherapies such as CD38 inhibitors
- chemotherapy
- corticosteroids.
Treatment for newly diagnosed myeloma is usually divided into three different phases:
- induction therapy, or front-line therapy, which normally consists of combinations of 3-4 different drugs, including an immunomodulatory agent, a proteasome inhibitor, a steroid, and in some cases, a CD38 inhibitor
- consolidation therapy, which normally involves a stem cell transplant if the patient is considered eligible; if not, induction therapy is continued
- maintenance therapy, which helps keep myeloma from recurring and normally involves the administration of an immunomodulatory therapy or a proteasome inhibitor.
Altogether, these three phases are considered one line of therapy.
Options for supportive care do not treat the underlying disease, but can help with symptom management and improve quality of life.
Every treatment option for myeloma comes with tradeoffs in terms of risks and benefits. For example, some therapies are very potent at killing myeloma but can cause serious side effects, whereas other medicines have milder safety profiles but aren’t always as effective.
When someone is diagnosed with myeloma, they will work with their care team to create a treatment plan, taking into account their specific situation. If one treatment regimen isn’t effective or is not tolerated, patients and their providers will often try other types of multiple myeloma treatment.
Stem cell transplant
Hematopoietic stem cells, or blood stem cells, are immature cells that possess the ability to differentiate into all types of blood cells, including plasma cells. A stem cell transplant is a procedure used in myeloma to restore the body’s capacity to generate healthy plasma cells. The patient receives new stem cells to replace the diseased or damaged ones in their bone marrow, effectively rebooting their blood cell production and promoting the generation of healthy cells.
A myeloma stem cell transplant is an intensive procedure that usually requires several weeks of hospitalization. Before the transplant, patients are treated with high-intensity chemotherapy and/or radiation to destroy any cancer cells and eliminate the existing stem cells in the patient’s bone marrow, making room for the transplanted cells to grow.
Healthy stem cells are then infused into the patient’s bloodstream, where they will travel to the bone marrow. Over the following few weeks, these transplanted cells will start to rebuild a new immune system.
The two main types of stem cell transplants:
- autologous, which uses a person’s own stem cells, is the most commonly used in myeloma
- allogeneic, which uses stem cells from a donor, is more rarely used.
Whether the stem cells come from the patient or from a donor, doctors will harvest stem cells from the bloodstream. This procedure is called a peripheral blood stem cell transplant.
A stem cell transplant is an invasive procedure, and the recovery usually takes several months. As such, this type of treatment is more commonly used for myeloma patients who are younger and otherwise healthy.
When a patient is undergoing a stem cell transplant, they often have low blood cell counts, which can increase the risk of serious infections and bleeding. Other potential side effects of a stem cell transplant include:
- fatigue
- nausea and vomiting
- diarrhea or constipation
- loss of appetite
- weight loss
- mouth sores.
If the blood stem cells come from a donor, a stem cell transplant can sometimes lead to graft-versus-host disease, a serious complication where the new blood cells start to attack the body’s own healthy cells.
Targeted therapy
Targeted therapies are medications commonly used for myeloma and target specific features of cancer cells or block specific biological processes that promote their growth and survival, thereby killing them.
The two main types of targeted myeloma therapy are immunomodulatory agents and proteasome inhibitors. Other types of targeted therapies may also be used in some cases.
Immunomodulatory agents
Immunomodulatory agents, often abbreviated IMiDs, are drugs that modulate the immune system. Although their exact mechanism of action is not entirely understood, they are thought to work by interfering with the growth and division of myeloma cells.
Examples of immunomodulatory agents that may be used in myeloma include:
- lenalidomide (sold as Revlimid and generics)
- pomalidomide (sold as Pomalyst and generics)
- thalidomide (sold as Thalomid and generics).
This type of targeted therapy is often given alongside aspirin or a blood thinner due to an increased risk of serious blood clots.
Proteasome inhibitors
The proteasome is a piece of molecular machinery that cells use to break down unneeded proteins into components that can be recycled to make new proteins. In cancer cells, the proteasome is usually very active, as the cells need to break down unwanted proteins to make new proteins and grow.
Proteasome inhibitors are medicines that block the activity of the proteasome, which causes a buildup of M protein and other unneeded proteins that ultimately kill the cancer cells.
Proteasome inhibitors used for myeloma include:
- bortezomib (sold as Velcade and generics)
- carfilzomib (sold as Kyprolis and generics)
- ixazomib (Ninlaro).
Other targeted therapies
Another type of targeted therapy that may be used in myeloma treatment are nuclear export inhibitors, which are medicines that can kill cancer cells by interfering with the movement of molecules out of the nucleus (the cellular compartment that houses DNA). A therapy in this class that’s approved for myeloma treatment is Xpovio (selinexor).
Histone deacetylase (HDAC) inhibitors are another class of targeted therapies used in myeloma that work by blocking proteins that control the genetic activity of cells, which can kill cancer cells. An HDAC inhibitor called Farydak (panobinostat) is approved for myeloma.
Another class of targeted therapies that may be used to treat myeloma are antibody-drug conjugates in which antibodies targeting proteins found on cancer cells are used to deliver toxic compounds to specifically kill those cells. One such therapy that is currently approved for multiple myeloma is Blenrep (belantamab mafodotin-blmf).
Side effects
While the safety profile varies widely from one medication to another, some common side effects of targeted therapies for myeloma may include:
- nausea and vomiting
- diarrhea or constipation
- low blood count
- numbness, tingling, and pain in the hands and feet
- blood clots
- fatigue
- weight loss and loss of appetite.
Immunotherapy
The immune system has the inherent ability to destroy cancer cells. However, cancers can often find ways to evade this defense mechanism. Immunotherapies aim to make the immune system more effective at targeting and eliminating cancer cells.
Different immunotherapy approaches can be used for myeloma, including:
- monoclonal antibodies
- bispecific T-cell engagers
- CAR T-cell therapies.
Monoclonal antibodies
Antibodies are proteins that the immune system normally makes to target threats. When an antibody binds to its target, it can directly kill its target cell and/or activate certain immune mechanisms to destroy the target.
Antibodies can also target proteins at the surface of certain immune cells to block mechanisms that would otherwise prevent them from destroying the cancer cells. These antibodies do not cause the death of their target cells; instead, they make immune cells more effective at targeting the cancer.
The main monoclonal antibodies used for myeloma include:
- Darzalex (daratumumab), which targets the CD38 protein found at high levels in plasma cells and directly causes their death while also triggering immune-mediated cell death.
- Sarclisa (isatuximab), another anti-CD38 antibody that works similarly to Darzalex.
- Empliciti (elotuzumab), which targets the SLAMF7 protein at the surface of myeloma cells and recruits specialized immune cells to kill the cancer cells.
Bispecific T-cell engagers
Bispecific T-cell engagers, or BiTEs, are lab-made antibodies that work by simultaneously binding one target on cancer cells and another on T-cells, which are a type of immune cell able to kill cancer cells.
By bringing the immune T-cells into close contact with the cancer cells, BiTEs essentially help the immune system attack the myeloma cells.
Three BiTEs are currently approved for myeloma:
- Elrexfio (elranatamab)
- Talvey (talquetamab)
- Tecvayli (teclistamab)
CAR T-cell therapies
CAR T-cell therapy involves collecting a patient’s own immune T-cells and modifying them with lab-made proteins called chimeric antigen receptors, or CARs. These modified T-cells are designed to specifically target and attack cancer cells. The engineered cells are then infused into the patient’s body to go after their cancer.
CAR T-cell therapies approved for myeloma include:
- Abecma (idecabtagene vicleucel)
- Carvykti (ciltacabtagene autoleucel)
These therapies are usually reserved for cases of myeloma that don’t respond well to other treatments.
Side effects
Side effects of immunotherapy for myeloma depend on the specific agent used, but may include:
- inflammatory reactions
- fever and headache
- nausea and vomiting
- diarrhea
- fatigue
- low blood cell counts
- liver problems
- muscle and joint pain
- rash
- weakness, numbness, and pain in the hands and feet.
Chemotherapy
Chemotherapy aims to kill cells that are growing rapidly. Because cancer cells are defined by excessive growth, chemotherapy can be an effective way to kill cancer cells.
Chemotherapy treatment for multiple myeloma is most commonly used to prepare patients for a stem cell transplant, but it can also be considered for patients whose disease failed to respond (refractory) to other treatments, or returned after an initial response (relapsed).
A variety of chemotherapy agents may be used as myeloma treatment drugs:
- cyclophosphamide (sold as Cytoxan and generics)
- melphalan (sold as Evomela, among others)
- bendamustine (sold as Treanda, among others)
- cisplatin
- doxorubicin (sold as Doxil and generics)
- etoposide.
These drugs are often given in combination with other therapies to maximize their cancer-killing potential. They may be administered orally or via a slow drip into the bloodstream.
While chemotherapy can be effective in eliminating cancer, its toxicity also extends to other healthy, fast-growing cells in the body, which can lead to several chemotherapy side effects that include:
- increased risk of infections
- fatigue and difficulty concentrating
- nausea and vomiting
- diarrhea or constipation
- loss of appetite
- sores in the mouth
- hair loss.
Other chemotherapy risks may include reduced fertility and a higher risk of future cancers.
Radiation therapy
Radiation therapy, also known as radiotherapy, uses high-energy X-rays aimed at specific areas where cancer is growing to kill cancer cells.
While radiation is often an important part of treatment for many cancers, it’s not a main therapy for multiple myeloma, unless there is only one spot where the cancer cells are growing.
Radiation is most commonly used in myeloma patients to manage bone problems caused by myeloma cells, especially if other treatments are not effective. By eliminating myeloma cells that are growing in specific areas, radiation can help lessen stress on bones and make room for bones to heal.
Radiation may sometimes be used to prepare for a stem cell transplant.
Side effects of radiation therapy can include:
- fatigue
- nausea or diarrhea
- low blood cell counts
- skin changes around the area being treated.
Corticosteroid therapy
Corticosteroids, also called glucocorticoids, are medications that work by mimicking the activity of cortisol, a hormone that the body makes naturally in response to stress.
At high doses, corticosteroids can suppress the growth of myeloma cells, but they can also decrease inflammation and reduce some of the side effects caused by other myeloma therapies, including targeted therapies and chemotherapy.
The most common corticosteroids used for myeloma include dexamethasone and prednisone, and they may be used on their own or in combination with other drugs at any point in the course of myeloma treatment.
Common side effects of corticosteroids include:
- weight gain
- high blood sugar
- mood changes
- difficulty sleeping.
Supportive therapies
In addition to treatments that target myeloma itself, patients often benefit from other therapies that can help ease the disease’s symptoms and complications.
Managing bone health
Because myeloma grows in the bone marrow, it can cause bone disease, leading to weakened bones and increasing the risk for fractures and broken bones. To manage bone disease, people with myeloma are commonly treated with medications that act to strengthen the bones.
The main bone-strengthening agents used in myeloma are bisphosphonates, a class of medicine that affects bone cells and helps prevent bone damage.
Surgery can also sometimes be used to repair or strengthen damaged bones, while radiation therapy can be used after surgery to repair a damaged bone.
Pain management
Myeloma can cause substantial pain, and many treatments can also cause pain as a side effect. The main medications used for pain management in myeloma are nonsteroidal anti-inflammatory drugs and opioids.
Radiation therapy can also be used to relieve bone pain.
Preventing infection
Myeloma can increase the risk of infections, and many of the treatments for the disease can also heighten infection risk. Infections in myeloma can be serious. In fact, infections are the most common cause of morbidity and mortality among myeloma patients.
Preventing infection is a key part of myeloma patient care, and include steps such as:
- minimizing contact with people who are sick
- using robust hygiene practices
- getting all recommended vaccines
- receiving prophylactic (preventive) treatments with specific anti-viral or anti-bacterial agents, especially in people at risk of certain infections.
Myeloma life expectancy with treatment
Myeloma can be a deadly disease, but current medical treatments have improved outcomes dramatically. Before 2000, the median life expectancy for someone with relapsed myeloma was about one year, but that increased to more than six years for patients diagnosed with myeloma in the early 2010s.
With the approval of more myeloma therapies in the last decades, and with new treatments becoming available, it’s expected that myeloma life expectancy will continue to increase. Clinical studies are ongoing to test new ways to treat myeloma and improve survival outcomes.
Currently, the five-year survival rate, or the percentage of people who are alive five years after diagnosis, is about 60% for multiple myeloma.
The prognosis of myeloma depends in large part on the disease stage. The five-year survival rate is:
- 82% for stage 1 myeloma, the mildest stage
- 62% for stage 2 myeloma
- 40% for stage 3 myeloma, the most severe stage. There is no stage 4.
Still, other factors such as age and co-occurring health issues can affect the prognosis of myeloma, and patients are advised to talk with their healthcare team about what’s realistic to expect in their specific situation.
Although many options are available to treat myeloma, there will be cases where the disease doesn’t respond well to any available therapy and progresses to the point that it becomes a terminal cancer. In these instances, supportive treatments such as palliative care and pain management usually become the focus of care to make patients as comfortable as possible.
Palliative care
Coping with myeloma can be difficult and emotionally taxing. Palliative care is a broad branch of medicine that focuses on maximizing quality of life for people with serious diseases.
Palliative care teams usually consist of various professionals, such as doctors, nurses, social workers, psychologists, and other experts. Patients may be referred to these teams for assistance in managing pain, dealing with side effects from treatment, and addressing any mental or physical distress they may be experiencing.
A common misconception is that palliative care is only for people who are close to death. While end-of-life care can be an aspect of palliative care in some instances, palliative care itself is more general and can be given to anyone dealing with a serious illness that affects their quality of life.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Preclinical study shows RNA therapy halts glioblastoma growth
- Ernexa’s stem cell therapy could soon enter ovarian cancer trials
- Scientists find new way to kill treatment-resistant myeloma cells
- Starting a new year with hope for myeloma treatment
- Phase 3 blood cancer vaccine trial moves toward final analysis
Related articles