Myeloma diagnosis: Tests and procedures
Last updated Oct. 23, 2025, by Lindsey Shapiro, PhD

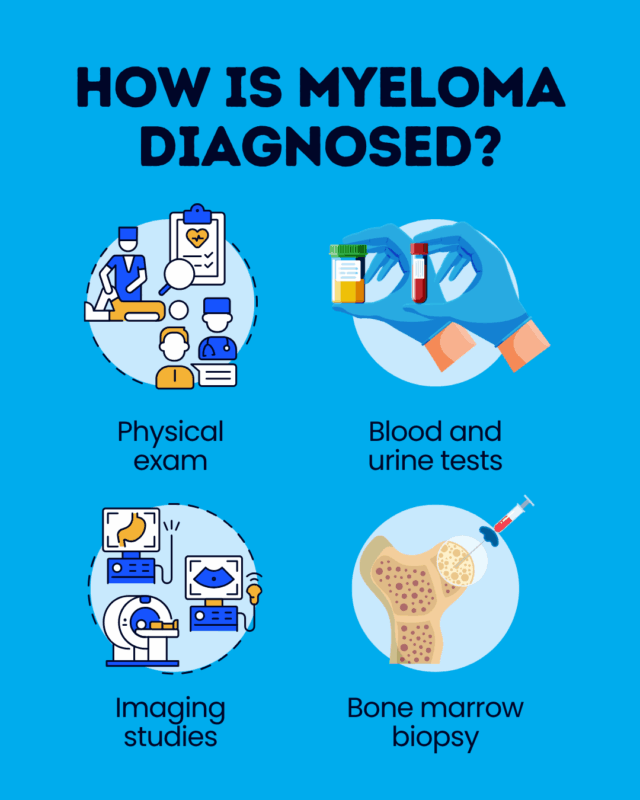
A diagnosis of myeloma is usually reached based on the collective results of a physical exam, blood and urine tests, bone marrow examination, and imaging studies.
Myeloma is a rare blood cancer caused by immune plasma cells that acquire genetic mutations and grow out of control in the bone marrow, the spongy center of bones where blood cells are made. While plasma cells usually make antibodies to help the body fight infection, cancerous myeloma cells produce an abnormal antibody called M protein.
Reaching an early and accurate myeloma diagnosis is key. It allows for earlier initiation of medications that can enhance overall prognosis and quality of life.
Importance of early diagnosis
It can be difficult to diagnose myeloma because the disease often does not cause symptoms in its early stages.
However, promptly recognizing the early signs of myeloma is critical for ensuring the best possible long-term outcomes.
Timely detection allows for the sooner start of myeloma treatments. While myeloma is generally considered incurable, advances in myeloma treatment and care have led to longer survival and better life quality for people with the blood cancer.
Initial clinical evaluation
In some cases, myeloma may be asymptomatic and the first signs of it are identified in blood tests done for other reasons. In other cases, a person may be experiencing symptoms that bring them to the doctor.
The first step in the myeloma diagnosis process will be to conduct a physical exam to look more closely for evidence of myeloma. Common findings physicians use to identify active, symptomatic myeloma may be summarized under the acronym CRAB:
- Calcium elevations in the blood (hypercalcemia), with symptoms of extreme thirst, appetite loss or nausea, constipation, or confusion
- Renal (kidney) failure, with symptoms like infrequent urination or leg swelling
- Anemia, or a lack of healthy red blood cells, leading to fatigue or weakness
- Bone problems, including pain, fractures, or weakness
Other possible signs of myeloma may include frequent infections due to a lack of healthy white blood cells, or easy bruising and bleeding due to a lack of platelets.
Diagnostic tests and procedures
If myeloma is suspected, several other tests will be run to establish whether the cancer is present and if so, what type it is and how advanced it is. Diagnostic tests for myeloma may involve:
- blood tests
- urine tests
- bone marrow analyses
- imaging studies
Blood and urine tests
Blood and urine tests for myeloma may be among the first tests that are performed.
Elevated levels of M protein in the blood, as measured by a test called serum protein electrophoresis, or in a urine sample, may be indicative of myeloma. Other antibodies, or antibody fragments called kappa and lambda free light chains, may also be measured. In myeloma, the balance of these antibodies may be disturbed.
Abnormal plasma cells crowd out other healthy blood cells in the bone marrow, including red blood cells, white blood cells, and platelets. A complete blood count can measure the levels of these cells, which are commonly lower than normal in a person with myeloma.
Blood tests for myeloma may also be used to look for:
- kidney dysfunction
- calcium levels, via a blood chemistry panel
- levels of proteins linked to disease prognosis and which are used for disease staging, including albumin, lactic dehydrogenase (LDH), and beta-2 microglobulin (B2M)
Bone marrow test
A bone marrow biopsy for myeloma usually includes:
- a bone marrow aspiration, to remove a liquid marrow sample
- a bone marrow biopsy, to collect a small piece of bone filled with marrow
A specialist will look at the size, shape, and appearance of cells in the collected sample to identify the presence and abundance of cancerous cells.
Myeloma cells will also be analyzed to look for underlying genetic abnormalities that are causing plasma cells to grow out of control. The specific type of genetic mutations that are found influences disease staging and prognosis.
Imaging
Imaging tests are a key part of diagnosing myeloma and determining how much it has spread. Positron emission tomography, or a PET scan, is used to create a detailed picture of where the cancer is located in the entire body. It is commonly combined with a CT scan, called a PET/CT.
Bone problems are very common in myeloma. A healthcare provider may also run X-rays or MRI scans to determine if a person has any signs of bone damage.
How is myeloma diagnosed
Collective results from these tests are used to diagnose myeloma. CRAB criteria used to be the standard, but more recent guidelines — sometimes called the SLiM CRAB criteria — allow for a diagnosis based either on the presence of myeloma symptoms or laboratory features that strongly suggest the disease will progress to active myeloma.
Current diagnosis criteria require that at least 10% of the bone marrow be made up of cancerous plasma cells or that a biopsy-proven plasma cell tumor (plasmacytoma) is present, in addition to at least one of the following:
- hypercalcemia
- poor kidney function
- anemia
- evidence of bone damage in imaging tests for myeloma
- bone marrow where at least 60% of cells are cancerous plasma cells
- at least a 100-fold difference in blood levels of kappa and lambda free light chains
If abnormal plasma cells or M protein are somewhat elevated but there are no clinical signs of myeloma and the diagnostic criteria are not met, a person may be diagnosed with one of two precancerous conditions that commonly precede myeloma, called monoclonal gammopathy of undetermined significance (MGUS) or smoldering myeloma.
These conditions may or may not progress to active myeloma, so people diagnosed with them need to be carefully monitored.
Diagnosis confirmation and staging
Once myeloma has been identified, doctors will stage the disease, that is, determine where it has spread and how quickly it is growing. This facilitates treatment planning.
There are multiple myeloma staging systems that may be used, but the one that’s usually favored is the Revised International Staging System (R-ISS), which considers four factors known to influence disease prognosis:
- B2M blood levels
- albumin blood levels
- LDH blood levels
- the specific genetic abnormalities in the cancer cells
Lower albumin levels, as well as higher B2M and LDH, are associated with a worse prognosis, as are certain types of genetic abnormalities.
From this, myeloma is categorized into three stages, numbered from 1-3, with stage 1 being the least aggressive and stage 3 being the most aggressive.
There are also a number of other factors that can influence a myeloma prognosis, and which a doctor may consider when deciding on a treatment plan, including age, kidney function, and overall health.
Distinguishing myeloma from other conditions
It is critical to distinguish MGUS and smoldering myeloma from active myeloma in the diagnostic process, as the monitoring and treatment approach differs. A lack of clinical symptoms as well as blood tests to measure levels of abnormal plasma cells and M protein can also help with the distinction.
Myeloma may also overlap with other plasma cell disorders:
- solitary plasmacytoma
- AL (light chain) amyloidosis, a condition linked to blood cancers where abnormal light chains produced from plasma cells build up and damage organs and tissues
- Waldenström macroglobulinemia, a cancer that’s characterized by overproduction of immunoglobulin M antibodies
Each of these conditions is treated differently, and as such, must be considered in the differential diagnosis of myeloma. Physicians can usually hone in on the right diagnosis by looking for the specific pattern of abnormal antibodies, protein buildup, and organ damage and related symptoms that characterize each disorder.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Inovio, Akeso partner on Phase 2 trial of new immunotherapy for glioblastoma
- My emergency go bag reflects my constant alertness as a caregiver
- Immune duo safely targets hard-to-treat gynecological cancers
- FDA approves Tecvayli, Darzalex Faspro in combo for hard-to-treat myeloma
- My fascination with celebrity cancer cases is not just morbid curiosity