Monoclonal gammopathy of undetermined significance (MGUS)
Last updated Oct. 31, 2025, by Lindsey Shapiro, PhD

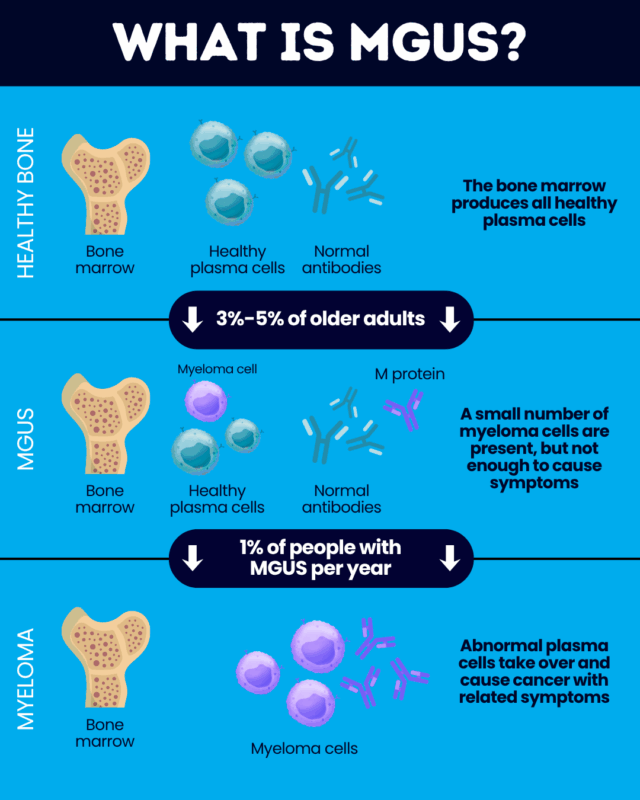
Monoclonal gammopathy of undetermined significance, or MGUS, is a noncancerous blood disorder that can sometimes progress to the rare blood cancer myeloma.
MGUS is relatively common in older people, affecting about 3% of individuals older than 50, and 5% of those older than 70. The disease doesn’t usually cause any obvious symptoms and most people don’t need to be treated.
But because a minority of people with MGUS will develop cancer or another serious blood disorder, the condition requires careful lifelong monitoring.
What is MGUS?
MGUS is a blood disorder characterized by a small population of identical — called monoclonal — plasma cells in the bone marrow, the spongy center of bones where blood cells are made. Plasma cells are a type of white blood cell that normally produce antibodies to help the body fight infection. The abnormal ones found in MGUS, however, produce an atypical antibody called monoclonal M protein.
The disease is part of a spectrum of related plasma cell disorders that includes myeloma, also called multiple myeloma because cancer cells may be found in more than one bone marrow location. It is important to understand the distinction between MGUS versus myeloma, as this has a substantial impact on treatment and prognosis.
In MGUS, the small numbers of abnormal M protein-producing plasma cells don’t generally cause any major problems. But in myeloma, these cells are found in larger amounts, completely crowding out other healthy blood cells and leading to various types of organ damage and related symptoms.
Smoldering multiple myeloma (SMM) is an intermediate condition in which there are more abnormal plasma cells growing than in MGUS, but not to the degree that causes the extensive damage seen in myeloma.
MGUS itself is not cancerous. But if the small number of abnormal plasma cells continues to grow out of control and start causing damage, it can progress to become myeloma. The disorder is thus understood to be a benign precursor to myeloma, and is among the key multiple myeloma risk factors.
Additionally, MGUS can progress to other types of blood cancers or serious disorders. These include:
- forms of lymphoma, such as Waldenstrom macroglobulinemia
- light chain amyloidosis, in which plasma cells produce misfolded antibody fragments (light chains) that accumulate in various organs and cause damage
Causes and risk factors
Myeloma cells exhibit various genetic abnormalities that are believed to drive their uncontrolled growth. Some of these genetic alterations may also be seen in MGUS-related plasma cells, although not as frequently.
As with myeloma, it is not exactly known why the body starts to produce abnormal plasma cells in MGUS, but the condition has been linked to certain risk factors. Among these are:
- older age, with MGUS being more common in people 50 and older
- male sex
- being of Black race
- having a close relative with MGUS or blood cancer
- a history of exposure to radiation or certain chemicals, such as pesticides or insecticides
These are generally the same factors that increase the risk of developing myeloma. Ongoing research is seeking to identify other factors that may be linked to these diseases.
Symptoms
MGUS rarely causes symptoms, and is usually diagnosed when blood or urine tests done for other reasons show elevated M protein levels.
Active myeloma, conversely, is associated with a range of symptoms, and their presence could suggest that MGUS has progressed to blood cancer. Such symptoms include:
- bone pain or other bone issues
- feeling extremely tired, short of breath, or unable to perform usual activities for no obvious reason
- frequent infections
- easy bruising or bleeding
- nausea, vomiting, appetite changes, or weight loss
- confusion
- constipation
- excessive thirst
- urinary changes
People who notice these or any other symptoms should talk with a healthcare provider who can run more tests to determine their cause.
Diagnosis
The hallmark of MGUS is elevated blood and urine levels of M protein, so tests to measure this — called urine or serum protein electrophoresis — are the main way of diagnosing the condition.
Blood tests will be used to look for signs of myeloma-associated damage, such as high blood calcium levels or kidney dysfunction. Other tests may also be done to rule out more serious conditions like myeloma if a person is considered to be at a higher risk.
- A bone marrow test, where a small sample of bone marrow is collected and analyzed under a microscope, can be used to see how many abnormal plasma cells are present.
- Imaging tests can be done to look for signs of cancer throughout the entire body.
According to current guidelines, three criteria must be fulfilled for MGUS to be diagnosed. They are:
- blood M protein concentrations less than 3 grams per deciliter g/dL)
- plasma cells accounting for fewer than 10% of bone marrow cells
- no myeloma-defining events, or signs or symptoms of myeloma-related organ damage
Signs of myeloma-related organ damage under these criteria include high blood calcium levels, kidney issues, bone problems, and anemia, indicated by low red blood cell counts.
These cutoffs are used to distinguish MGUS from smoldering and active myeloma. Higher M protein concentrations and/or plasma cell levels in the absence of myeloma symptoms may meet the criteria for SMM.
Once abnormal plasma cells are at least 10% in the bone marrow and there is at least one myeloma-defining event — clinical signs of the cancer or biomarkers suggesting progression to myeloma is inevitable — this warrants a myeloma diagnosis.
Risk of progression to myeloma
The relationship between MGUS and myeloma is complex: Virtually all people with myeloma have MGUS first, but only a minority of people with MGUS go on to develop myeloma.
Approximately 1% of people with MGUS develop myeloma or another serious blood disorder each year, and about a quarter of people with the noncancerous condition will progress to something more serious at some point in their lives.
To determine a person’s risk of progression, healthcare providers will look at a few factors, including:
- the amount of M protein in the blood, with higher levels linked to a greater risk
- the type of M protein in the blood, with certain subtypes of the abnormal protein associated with the development of more serious disorders
- the amount of free light chains in the blood, with an abnormal ratio of these antibody fragments associated with a higher blood cancer risk
Doctors will use that information to determine if a person is at a low, intermediate, or high risk of progression, which dictates how often and in what ways a person with MGUS needs to be monitored. Routine blood and urine tests to keep track of M protein levels are standard, but individuals at higher risk may also need bone marrow biopsies or imaging.
There is, as of now, no way to prevent MGUS from progressing to myeloma. Adhering to an appropriate monitoring plan is key to ensuring that, should myeloma or other serious conditions arise, they are detected and treatment can be started as soon as possible.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Daily pill to stop pancreatic cancer spread granted FDA orphan drug status
- How to practice being an imperfect (but compassionate) caregiver
- New cell therapy for glioblastoma doubles progression-free survival
- Oral treatment for ovarian cancer put on FDA fast track
- J&J seeks approval in EU of Tecvayli-Darzalex for hard-to-treat myeloma
