Myeloma causes and risk factors
Last updated Oct. 21, 2025, by Lindsey Shapiro, PhD

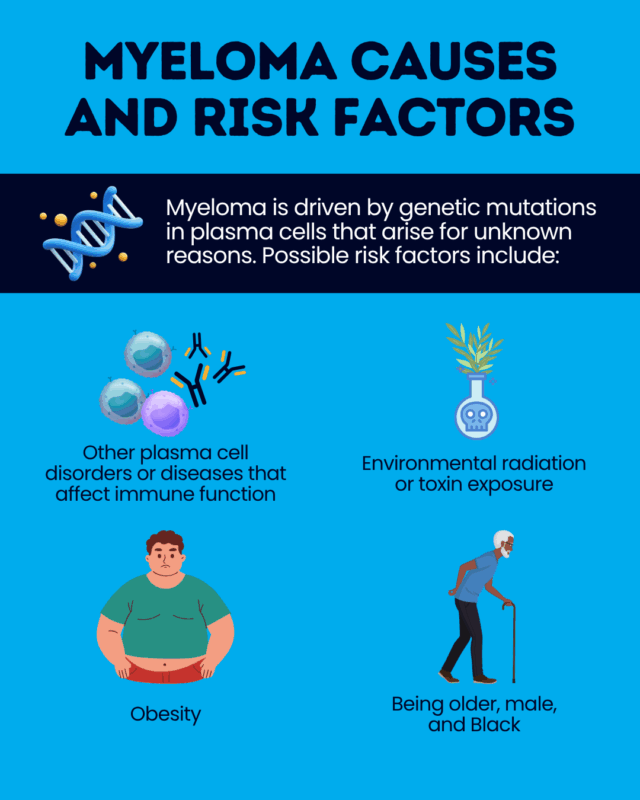
The exact cause of myeloma is not known, and in most cases, there is no obvious reason why this rare blood cancer develops.
Myeloma, often referred to as multiple myeloma, occurs when plasma cells — the antibody-producing white blood cells that normally help the body fight off infections —grow out of control in the bone marrow, which is the spongy tissue at the center of the bones where blood cells are made.
These myeloma cells don’t function the way normal plasma cells do, and produce an abnormal antibody called M protein. They crowd out healthy blood cells, leading to a range of severe symptoms and complications such as bone pain, kidney problems, and infections.
As with other cancers, myeloma is believed to arise when plasma cells acquire genetic mutations that cause them to become cancerous and grow uncontrollably. There are a variety of environmental, demographic, and health-related risk factors that may contribute to this process.
Many myeloma risk factors are beyond a person’s control, and there is no definitive strategy for myeloma prevention. Still, understanding myeloma causes can help individuals manage modifiable risk factors and be aware of their individual need for monitoring to enable early disease diagnosis and treatment.
Genetic factors
Multiple myeloma arises due to genetic mutations in plasma cells that occur spontaneously and generally do not have a known trigger.
There is no single genetic cause of myeloma, and numerous genetic abnormalities have been implicated in the disease. These genetic alterations often impair processes that normally regulate how cells grow, divide, and survive, ultimately allowing the plasma cells to grow out of control.
Most myeloma patients have one or more abnormalities in their chromosomes, the structures that carry DNA. This can include:
- deletions, a loss of all or part of a chromosome
- duplications, or gains, meaning extra copies of all or part of a chromosome
- translocations, or abnormal exchanges of genetic material between chromosomes
Mutations in specific cancer-related genes can also be observed, including in the following genes:
- KRAS
- NRAS
- BRAF
- MYC
- TP53
Because these genetic abnormalities occur randomly, myeloma is not overall considered a hereditary condition, and most people with the disease do not have a family history of multiple myeloma.
However, this blood cancer does sometimes run in families, and having a sibling or parent with myeloma is considered a risk factor. However, this could stem from a combination of shared environmental and genetic factors.
Environmental and lifestyle factors
Certain environmental, lifestyle, and occupational risks are linked to myeloma, including:
- exposure to radiation
- exposure to chemicals such as pesticides, fertilizers, herbicides (including Agent Orange), and organic solvents
- being overweight or obese
People who have occupational exposures to radiation or myeloma-associated chemicals may be at a particular risk, specifically, individuals who work in agricultural or industrial sectors. First responders in some areas are also found to be at an increased risk.
Exactly how these factors may cause myeloma is not known, but it is possible that they contribute to cellular or DNA damage in plasma cells that drive the disease.
Age, sex, and ethnicity
Various demographic factors may contribute to the risk of myeloma, including:
- age, with most people who develop myeloma being older than 65
- sex, with men being more likely to develop myeloma than women
- race, with myeloma being twice as common in Black people as in white people
Genetic changes that accumulate over a person’s lifetime may be one reason that myeloma occurs more often in older people. The exact reasons why the disease happens more in men and Black people have not been established.
Preexisting conditions and immune system factors
People who have other diseases that affect plasma cells are at risk of progression to multiple myeloma.
Active myeloma is almost always preceded by at least one of two precancerous conditions that are characterized by some elevation in plasma cells but which do not meet the diagnostic criteria for myeloma. Not all people with these disorders will go on to develop myeloma.
- Monoclonal gammopathy of unknown significance (MGUS) is an early precancerous condition in which plasma cells are slightly increased in the bone marrow. About 1% of people with MGUS develop myeloma each year.
- Smoldering myeloma is an intermediate stage between MGUS and myeloma, characterized by 10%-60% plasma cells in the bone marrow. About 10% of people with this condition will develop myeloma each year.
Solitary plasmacytoma is a very rare blood cancer marked by a single mass of abnormal plasma cells (a plasma cell tumor) in the bone, bone marrow, or soft tissues. It can also progress to myeloma. As many as 70% of people with plasmacytoma will develop multiple myeloma, with the risk at its greatest when the plasmacytoma affects bone tissue.
The risk of developing multiple myeloma may also be higher in people with conditions that affect immune system function. This includes individuals with weakened immune systems or those who are chronically immunosuppressed, such as those with HIV/AIDS or who are taking immunosuppressive medications, as well as people with the autoimmune disease pernicious anemia.
Emerging risk factors
Despite recent advances in the understanding of myeloma, exactly why plasma cells acquire cancer-driving mutations in the disease is not fully established.
Scientists are still working to identify as yet undiscovered risk factors that could contribute to myeloma. They’re also aiming to understand how certain established risk factors — such as race and environmental exposures — specifically contribute to the disease.
A better understanding of multiple myeloma causes will enable scientists to create new, more targeted therapies for treating the rare blood cancer in the future.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- How to travel from fear to hope on our myeloma journey
- FDA gives green light to first human trial testing cancer drug GTB-5550
- No one prepared me for the unwritten rules of caregiving
- Scientists test treatment strategy using ‘glioblastoma on a chip’
- Prostate cancer tool may cut risk for women in radiation therapy
