Treatments for blood cancers
Last updated Dec. 18, 2024, by Marisa Wexler, MS

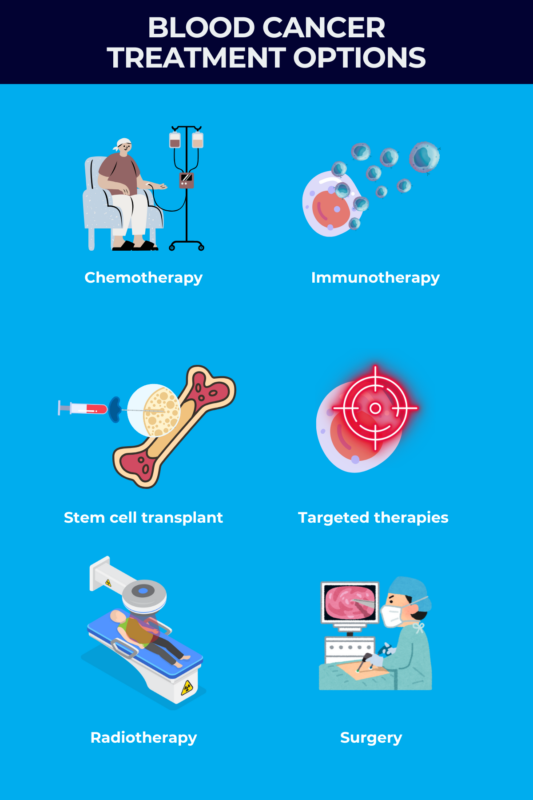
A wide range of therapies are available for treating blood cancer, from chemotherapy and targeted therapy to radiation, stem cell transplant, and surgery.
When devising a suitable treatment plan for blood cancer, healthcare providers take into account various factors, such as age, overall health, the specific type of blood cancer, and potential treatment side effects.
This tailored approach helps determine the most appropriate treatment or combination of treatments, ultimately optimizing the blood cancer survival rate.
It is crucial for people with blood cancer to talk with their healthcare team to create a personalized treatment plan that addresses their unique circumstances, ensuring the best possible outcomes.
Blood cancer types
Blood cancers result from the abnormal and uncontrolled proliferation of blood cells due to mutations in these cells’ DNA. The bone marrow serves as the primary site for the development and maturation of all blood cells, which then enter the bloodstream to perform various functions throughout the body.
Treatment plans vary depending on the types of blood cancer and their characteristics, with some types being more challenging to manage than others. However, across all types, blood cancer life expectancy with treatment significantly improves with appropriate care compared to no treatment at all.
Developing a tailored treatment plan based on the particular blood cancer diagnosis will help optimize outcomes and enhance overall survival.
Leukemia
Leukemia, the most common form of blood cancer, is caused by the uncontrolled growth of immature blood cells in the bone marrow. In leukemia, the cancer cells are found distributed through the bloodstream and generally do not form solid masses, or tumors.
Leukemia can be classified based on its progression rate and the specific blood cell type affected. The four primary types of leukemia are:
- acute lymphocytic leukemia (ALL)
- acute myeloid leukemia (AML)
- chronic lymphocytic leukemia (CLL)
- chronic myeloid leukemia (CML)
Lymphoma
Lymphoma is caused by the uncontrolled growth of white blood cells in the lymphatic system, mainly the lymph nodes, which are organs that house white blood cells. Unlike leukemia, lymphomas do form solid tumors.
Lymphomas are commonly classified as either:
- Hodgkin lymphoma, typically affecting younger adults or those over 65
- non-Hodgkin lymphoma, normally affecting older adults.
Myeloma
Myeloma is caused by the uncontrolled growth of a specific type of white blood cell, called plasma cells, in the bone marrow. These cells are responsible for producing antibodies, proteins that are used to fight infections.
Myeloma is often referred to as multiple myeloma because it typically affects more than one part of the body at once.
Creating a treatment plan
When someone receives a blood cancer diagnosis, their care team will work with them to create a treatment plan. Cancer care often requires a multidisciplinary team of healthcare professionals to address a patient’s specific needs based on their cancer type and stage. This collaborative approach may involve various specialists, such as surgeons, pathologists, medical and radiation oncologists, rehabilitation experts, palliative care providers, pharmacists, nurses, dietitians, social workers, and case managers.
There are different types of therapies available for blood cancer treatment and each carries potential benefits and risks. Sometimes, a treatment plan will involve very aggressive therapy from the onset, but other times it will involve watchful waiting to monitor the cancer and see if any treatment is required. These decisions depend on each individual’s situation and blood cancer prognosis. Often, different types of treatment will be used as part of one person’s treatment plan.
Many aspects of the treatment plan will be determined based on the individual’s specific cancer and its progression rate. Doctors will also consider a person’s overall health and age when making recommendations about treatment plans, because many cancer treatments can be very rough on the body and some can lead to serious or even fatal complications.
Patients may also wish to consider engaging in blood cancer research, such as participating in clinical studies for experimental therapies. Ultimately, the decision about which treatment(s) to use should be left up to the patient.
Chemotherapy
Chemotherapy uses powerful medications that target and disrupt the proliferation of rapidly-dividing cells, a characteristic feature of cancer cells. By exploiting this weakness, chemotherapy can effectively eliminate cancer cells. Although chemotherapy may also affect some healthy cells, its potency against malignant cells makes it a mainstay cancer treatment.
Chemotherapy may be used as part of leukemia treatment, lymphoma treatment, and myeloma treatment. It can also be used to help make other treatments more effective.
There are many different types of chemotherapy for blood cancer; most are given via an infusion into the bloodstream, though some are taken taken by mouth as a pill. Often, multiple different chemotherapy drugs are combined in order to maximize the cancer-killing potential. There are dozens of different chemotherapies available; the choice of which specific medication(s) to use will depend on factors like the specific cancer subtype.
Commonly used chemotherapy agents to treat blood cancer include:
- bendamustine hydrochloride (brand names Bendeka, Treanda, among others)
- Leukeran (chlorambucil)
- Cytoxan (cyclophosphamide)
- daunorubicin (brand names Cerubidine, Vyxeos)
- Doxil (doxorubicin)
- Mavenclad (cladribine)
- melphalan (brand name Evomela, among others)
- Mylotarg (gemtuzumab ozogamicin)
- midostaurin (sold as Rydapt and generics)
- Vyxeos (daunorubicin and cytarabine).
Sometimes chemotherapy agents are given in combination with other types of therapies, such as immunotherapies and corticosteroids. For example, R-CHOP is a commonly used treatment for a type of aggressive lymphoma that combines rituximab (brand names Rituxan, among others), cyclophosphamide, doxorubicin, vincristine and prednisone.
Although it kills cancer effectively, chemotherapy also is toxic to other rapidly growing cells in the body, including cells that make hair and cells in the digestive tract. Chemotherapy side effects often include:
- hair loss
- digestive issues like nausea and diarrhea
- fatigue
- weight changes
- mood abnormalities.
Other chemotherapy risks can include fertility problems, neurological damage, and increased susceptibility to infection.
Immunotherapy
The body’s immune system is equipped to be able to kill cancer cells, but cancers will typically develop ways to avoid immune-mediated destruction. Immunotherapies are a class of treatment that seeks to unleash the immune system to go after cancer cells and kill them more effectively.
There are several different types of immunotherapy that may be used to treat blood cancers, the most common of which include antibody-based treatments and adoptive cell therapies. Immunotherapy, typically administered via infusions into a vein, or intravenously, or injectionos under the skin, that is, subcutaneously, may be used in combination with other cancer treatments, after chemotherapy to prevent cancer recurrence, or as a standalone therapy.
Antibodies are proteins made by the immune system to help target threats. Monoclonal and bispecific antibodies are lab-made antibodies designed to target one or more particular proteins. As a cancer treatment, lab-made antibodies can direct the immune system to go after cancer cells by targeting proteins that are expressed by these cells. There are also antibody therapies that work by attaching an antibody to a toxin or radioactive molecule, allowing the antibody to deliver the drug directly to cancer cells.
Some commonly used antibody-based treatments for blood cancer include:
- alemtuzumab (sold as Campath, Lemtrada)
- Besponsa (inotuzumab ozogamicin)
- Blincyto (blinatumomab)
- Darzalex (daratumumab)
- Mylotarg (gemtuzumab ozogamicin)
- rituximab.
Adoptive cell therapies are another type of immunotherapy that involves the infusion of immune cells into the patient to fight cancer. In some cases, these therapies leverage immune cells sourced from a healthy donor, as they may better recognize and eliminate cancer cells.
Perhaps the most well-known type of adoptive cell therapy are CAR T-cells, which use immune cells called T-cells equipped with lab-made proteins called chimeric antigen receptors, or CARs, to go after a specific target. CAR T-cell therapy is generally considered as a treatment option when other conventional therapies have proven ineffective or unsuccessful, and is often used as a later line of treatment.
Some commonly used CAR-T cell therapies include:
- Abecma (idecabtagene vicleucel)
- Aucatzyl (obecabtagene autoleucel)
- Breyanzi (lisocabtagene maraleucel)
- Carvykti (ciltacabtagene autoleucel)
- Kymriah (tisagenlecleucel)
- Tecartus (brexucabtagene autoleucel)
- Yescarta (axicabtagene ciloleucel).
Antibody treatments and CAR T-cells are only able to work if cancer cells express one or more proteins that can be targeted by the antibody or the CAR. As such, these treatments are generally only given after testing to confirm the patient has a cancer that is likely to respond.
In addition to targeted immunotherapies, sometimes cytokines – naturally-occurring signaling molecules that stimulate and enhance the immune system’s attack on threats – may be administered as part of treatment for blood cancer.
Because all immunotherapies work to activate the immune system, some side effects that can occur whenever the immune system is activated include:
- fever and flu-like symptoms
- tiredness
- headache and nausea
- shortness of breath
- drop in blood pressure
- irregular heartbeat
- chest pain
- low blood cell counts.
Some immunotherapies also can cause serious or even life-threatening inflammatory reactions, so it’s important to discuss the potential risks with each specific therapy before initiating treatment.
There are also several types of immunotherapy that are currently in investigational stages, such as cancer vaccines that aim to teach a patient’s immune system to more efficiently target cancer cells.
Stem cell transplant
A stem cell transplant, commonly referred to as a bone marrow transplant, is a procedure designed to restore the body’s ability to produce healthy blood cells. The bone marrow houses stem cells, which have the unique capacity to develop into various types of blood cells, such as red blood cells, white blood cells, and platelets.
In a blood cancer stem cell transplant, a patient receives new stem cells to replace the diseased or damaged ones in their bone marrow, effectively rebooting their blood cell production and promoting the generation of healthy cells.
Before the transplant, high doses of chemotherapy and sometimes radiotherapy are necessary to prepare the body for the transplant. This is called “conditioning treatment” and can be very harsh on the body and lead to severe side effects.
There are two main types of stem cell transplants:
- autologous, which uses a person’s own stem cells
- allogeneic, which uses stem cells from a donor.
A stem cell transplant may be used as part of leukemia, lymphoma, and myeloma treatment. Not everyone will be eligible for this procedure, however, and a doctor will usually consider a person’s general health, the type and stage of the blood cancer, previous medical treatments, and the ability to use a person’s own stem cells or the availability of a matching donor.
In general, outcomes from stem cell transplant are usually better when the procedure is performed early on in the course of disease.
Targeted therapies
Blood cancers occur when specific blood cells undergo abnormal and uncontrolled growth. This typically happens due to disruptions in the molecular signaling pathways that usually regulate cell growth and division. When these pathways malfunction, they can erroneously signal cells to grow and multiply even when they should not.
Targeted therapies are medicines that block the activities of specific molecular pathways to stop the growth of cancer cells, often killing them in the process. A common class of targeted therapies are tyrosine kinase inhibitors, or TKIs. Tyrosine kinases are a broad category of signaling proteins involved in many cell growth pathways.
Some common targeted therapies include:
- Bosulif (bosutinib)
- imatinib (sold as Gleevec, Imkeldi)
- Imbruvica (ibrutinib)
- Scemblix (asciminib)
- nilotinib (sold as Tasigna, Danziten)
- Venclexta (venetoclax)
- Zydelig (idelalisib).
Targeted therapies are only effective in cancers where cell growth is driven by the specific molecular pathway that the therapy targets, so analyses of a patient’s cancer is usually necessary to determine what, if any, targeted therapies may be appropriate in their particular situation.
Because these medications target a specific pathway, they are often better tolerated than chemotherapies that more broadly kill rapidly growing cells. However, some targeted therapies can still cause serious side effects, including:
- diarrhea
- nausea
- muscle pain
- fatigue
- skin rashes
- swelling around the eyes, hands, or feet.
Targeted therapies are typically taken by mouth or via infusion into the bloodstream.
Radiotherapy
Radiotherapy, also known as radiation therapy, uses high-energy beams (radiation) to kill cancer cells. When cells divide, they become vulnerable to damage from radiation, and because cancer cells are by definition rapidly dividing, they are especially susceptible to damage from radiation.
Radiotherapy for blood cancer typically uses a machine that will blast beams of radiation at specific points in the body. Doctors will determine exactly how much radiation and where to aim it based on the layout of a person’s particular cancer.
Because lymphomas are marked by solid tumors, radiotherapy is often a key part of both Hodgkin lymphoma and non-Hodgkin lymphoma treatment.
While radiotherapy alone may not provide a cure for blood cancer, it can be combined with other types of treatment and can also be used to relieve symptoms and improve quality of life.
Common radiotherapy side effects include:
- fatigue
- skin damage
- damage to the area of the body that’s receiving radiation (for example, radiation near the mouth can cause dry mouth or mouth sores, whereas radiation in the abdomen may cause nausea or diarrhea).
There may also be long-term radiotherapy risks, such as:
- infertility
- heart disease
- skin changes
- cognitive problems
- increased risk of developing other cancers.
The extent of these risks will depend on how much radiation is administered and to what part of the body.
Surgery
Surgery may be used to treat some types of lymphoma if there is a clearly defined tumor that has not spread to other parts of the body. In these cases, the goal of surgery is to remove the tumor, effectively eliminating the cancer from the body. However, surgery is usually not the first choice of treatment; typically other interventions like radiation therapy are preferred because they aren’t as invasive.
Surgery is not typically a treatment option for leukemia or myeloma because there is not a solid mass of cancer cells that can be surgically removed. In some people with these blood cancers, surgery may be performed to insert catheters (tubes) that make it easier to administer treatments like chemotherapy, or to help manage complications of blood cancers such as broken bones, spinal cord compression, or enlarged spleen, but these types of blood cancer surgery are for management and do not treat the underlying cancer itself.
Other treatments
Treatments like chemotherapy, immunotherapy, and radiation are used to treat blood cancer itself. But people with blood cancer often require other treatments to help manage the symptoms of blood cancer and the side effects of therapy.
For example, blood cancers and their treatments can often lead to too low levels of healthy blood cells, in which case a blood transfusion may be used to restore blood cell counts.
There are also various therapies that can be used to manage treatment side effects, ranging from anti-nausea medicines to antidepressants. Patients experiencing unpleasant side effects are advised to talk to their providers about possible options for side effect management.
People with blood cancer may also benefit from palliative care, which is a broad branch of medicine that aims to support an individual’s comfort.
Palliative care is often mistaken as a form of care exclusively for those nearing the end of life. However, it is intended for anyone undergoing physically and emotionally challenging medical treatments, aiming to improve their quality of life throughout their healthcare journey, regardless of their life expectancy.
Lifestyle changes
Getting a diagnosis of any type of cancer can be terrifying and stressful, but there are steps that can be taken to make living with blood cancer as manageable as possible. Tips for living well with blood cancer include:
- Communicating open and honestly with healthcare providers, being clear about desires and asking for help wherever it’s needed.
- Talking with family and friends, and leaning on others for support.
- Connecting with others in the blood cancer community and taking advantage of resources like patient organizations and support groups. For example, the Leukemia and Lymphoma Society offers many support groups for people with blood cancer in the U.S.
- Eating a well-balanced diet and drinking plenty of fluids.
- Finding ways to stay active and exercise where possible. Healthcare providers and patient organizations can be useful resources for finding ways to safely exercise while undergoing cancer treatment.
- Prioritizing rest and allowing the body time to heal.
- Practicing self-care wherever possible.
- Reaching out for financial support if needed, and trying to prioritize health over working.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Clearnote’s blood test uses AI to spot pancreatic cancer in high-risk groups
- Being a caregiver requires constant, sometimes impossible, calculations
- Immuno-gene therapy for brain cancer tumors now on FDA fast track
- FDA approves Keytruda for hard-to-treat gynecological cancers
- FDA reviewing new iberdomide combo for hard-to-treat multiple myeloma
Related articles