
Sarclisa (isatuximab-irfc) for multiple myeloma
Last updated Oct. 28, 2024, by Marta Figueiredo, PhD

What is Sarclisa for multiple myeloma?
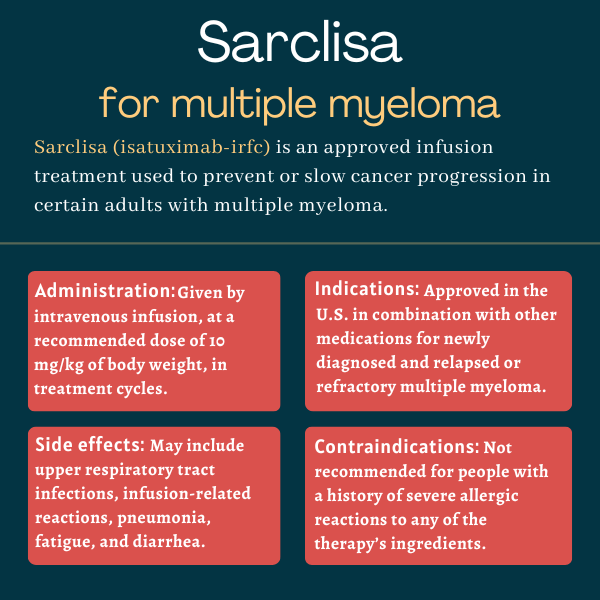
Sarclisa (isatuximab-irfc) is an infusion treatment approved for adults with multiple myeloma. In the U.S., the therapy is used in combination with other anti-cancer medications across several populations, from newly diagnosed patients to those with relapsed or refractory disease who have received several previous lines of treatment.
Administered via an intravenous, or into-the-vein, infusion, Sarclisa is designed to help bring myeloma under control or slow its progression by targeting a protein at the surface of myeloma cells.
It was originally developed by Immunogen and later licensed to Sanofi, which is also developing Sarclisa as a potential treatment for other blood cancers, including certain lymphomas.
Therapy snapshot
| Brand name: | Sarclisa |
| Chemical name: | Isatuximab-irfc |
| Usage: | Used as an early and late line of therapy in combination with other treatments; may help to slow or halt cancer progression |
| Administration: | Intravenous infusion |
How does Sarclisa work?
Multiple myeloma is a rare blood cancer in which plasma cells, a type of immune cell, grow uncontrollably in the bone marrow, where blood cells are formed. Instead of producing antibodies that help the body fight infections and other threats, cancerous plasma cells, or myeloma cells, produce an abnormal antibody called M protein.
The accumulation of myeloma cells within the bone marrow limits the natural growth of other types of blood cells and damages the bone. These cells can also spread through the bloodstream to form tumors in other parts of the body, damaging other tissues and organs.
This gives rise to a range of myeloma symptoms, such as blood abnormalities, kidney issues, and neurologic problems.
Many treatment options are available for multiple myeloma, but this cancer is often refractory, meaning it does not respond to such therapies, or has relapsed, meaning it comes back after treatment initially resulted in disease remission.
Sarclisa, previously known as SAR-650984, belongs to a class of medicines known as CD38 inhibitors. It is a lab-made antibody designed to bind to CD38, a receptor protein found at high levels at the surface of myeloma cells. This binding promotes the cells’ death through several mechanisms.
By destroying myeloma cells, Sarclisa is expected to help slow or halt myeloma progression.
Who can take Sarclisa?
Sarclisa was first approved by the U.S. Food and Drug Administration (FDA) in March 2020, but its label was then expanded in 2021 and 2024 to include additional indications. The therapy is now approved in the U.S. to be used:
- in combination with Pomalyst (pomalidomide) and dexamethasone for adults with relapsed or refractory multiple myeloma (RRMM) who have received at least two previous lines of therapy, including lenalidomide (sold as Revlimid, with generics available) and a proteasome inhibitor (PI).
- in combination with Kyprolis (carfilzomib) and dexamethasone for adult RRMM patients who received one to three prior lines of therapy.
- in combination with a standard first-line treatment regimen known as VRd, which combines bortezomib (sold as Velcade, with generics available), lenalidomide, and dexamethasone, for adults with newly diagnosed multiple myeloma who are not eligible for autologous stem cell transplant (ASCT), a type of transplant that uses patients’ own stem cells to repopulate the bone marrow.
The latest decision made Sarclisa the first anti-CD38 therapy used in combination with the standard VRd regimen to be cleared for newly diagnosed myeloma patients who are ineligible for ASCT.
Those prescribed the therapy in the U.S. may be eligible to enroll in Sanofi’s CareASSIST Patient Support program, which provides reimbursement and financial support, and other information.
Sarclisa is also approved for similar indications in adults with RRMM in more than 50 other countries, including Canada and the European Union.
Who should not take Sarclisa?
Sarclisa is contraindicated, or not recommended, for anyone with a history of severe allergic reactions to isatuximab or any other ingredient in the medication.
How is Sarclisa administered in multiple myeloma?
Sarclisa is administered by a healthcare provider via an infusion directly into the bloodstream, at a recommended dose of 10 mg per kilogram of body weight.
It is available in single-dose vials containing 20 mg of the active therapy per mL of a clear to slightly opalescent, colorless to slightly yellow solution. The exact amount of medication being infused will be determined prior to each dose based on the person’s weight.
Treatment cycles typically last about four weeks, and Sarclisa is administered once a week in the first cycle and every other week in subsequent cycles. Exceptions involve the Sarclisa-VRd combo for newly diagnosed patients, in which the first four treatment cycles last six weeks and Sarclisa is given once every four weeks in cycles 18 and beyond.
Infusion times become shorter as treatment advances, lasting about three hours and 20 minutes in the first infusion, nearly two hours in the second, and one hour and 15 minutes in subsequent infusions.
About 15 minutes to one hour before each Sarclisa infusion, patients should receive medications to reduce the risk and severity of infusion-related reactions. These include the corticosteroid dexamethasone, the fever-reducing medication acetaminophen, and antihistamines.
When a scheduled Sarclisa dose is missed, an infusion should be given as soon as possible, and the treatment schedule must be adjusted accordingly to maintain the recommended treatment interval.
Sarclisa in clinical trials
Sarclisa’s approvals in the U.S. were each supported by data from a global Phase 3 clinical trial. In all three trials, the main goal was to assess whether the Sarclisa combination could extend progression-free survival (PFS), or the time a person lives without signs of disease progression, compared with standard treatment without Sarclisa.
Secondary goals included differences in rates of treatment response, minimal residual disease (MRD) negativity, overall survival, and safety profiles. MRD refers to the small number of myeloma cells that may remain after treatment and cause a relapse.
ICARIA-MM
The approval of the Sarclisa, Pomalyst, and dexamethasone combination for RRMM patients was based mainly on data from the Phase 3 ICARIA-MM study (NCT02990338).
The trial enrolled 307 patients who had received at least two prior lines of therapy, including lenalidomide and a PI. Participants were randomly assigned to receive either Sarclisa plus the standard combination of Pomalyst and low-dose dexamethasone, or the standard combo alone (control group) until they experienced disease progression or unacceptable toxicity.
Results after a median of 11.6 months showed that the Sarclisa combo significantly prolonged PFS by about five months relative to standard treatment (11.5 vs. 6.5 months). This reflected a 40% reduction in the risk of disease progression or death with Sarclisa.
A significantly greater proportion of Sarclisa-treated patients showed at least a partial response compared with those on Pomalyst and low-dose dexamethasone alone (60% vs. 35%).
Longer-term data, at a median of nearly three years, demonstrated that the Sarclisa combo was still associated with a 40% lower risk of disease progression or death. It also significantly lowered the risk of death by 24%, with Sarclisa-treated patients living a median of 24.6 months compared with 17.7 months for the control group.
MRD negativity was reported in 10 Sarclisa-treated patients (7%) and none of those given standard treatment, also supporting the superiority of the combination.
IKEMA
The approval of Sarclisa, in combination with Kyprolis and dexamethasone (Kd), for RRMM patients was mostly supported by interim results from the Phase 3 IKEMA trial (NCT03275285).
The study tested the triple combo against Kd alone in 302 adults with RRMM who had received one to three previous lines of treatment. Treatment was administered in four-week cycles until disease progression or unacceptable toxicity occurred.
Interim findings at a median follow-up of 20.7 months (a little over 1.5 years) showed that PFS was 19.15 months for the Kd combo group but had not yet been reached in the Sarclisa group, indicating that most of these patients were still free from signs of cancer progression. This represented a 45% lower risk of disease progression or death with the Sarclisa combo.
Compared with those on Kd only, a significantly higher proportion of Sarclisa-treated patients achieved a response deemed “very good” or better (72.6% vs. 56.1%) and MRD negativity (29.6% vs. 13%).
Updated results after a median follow-up of about 3.5 years showed that Sarclisa extended patients’ PFS by about 1.5 years relative to the standard Kd combo, reflecting a 42% reduction in the risk of progression or death with Sarclisa.
In this long-term analysis, those treated with Sarclisa were significantly more likely to achieve a complete response or stringent complete response, meaning no detectable cancer, compared with those given the Kd regimen (44.1% vs. 28.5%). Sarclisa was also significantly superior at helping patients achieve MRD negativity (33.5% vs. 15.4%).
IMROZ
The clearance of the Sarclisa-VRd combo for newly diagnosed patients was based mainly on results from the Phase 3 IMROZ trial (NCT03319667). The study enrolled 446 patients who were not eligible for a stem cell transplant because of older age or concurrent health conditions. Participants were randomly assigned to receive either the Sarclisa-VRd combo or VRd alone.
Results after a median follow-up of nearly five years showed that patients on the VRd combo had a median PFS of 54.3 months, or about 4.5 years, whereas this estimate had not yet been reached in the Sarclisa group. This reflected a 40% lower risk of disease progression or death with Sarclisa.
Sarclisa treatment was also linked to significantly higher rates of complete response or better, meaning no detectable myeloma in blood or urine tests (74.7% vs. 64.1%), and MRD negativity (55.5% vs. 40.9%).
Ongoing trials
Several clinical trials are underway to evaluate Sarclisa for other possible indications in multiple myeloma. Sanofi also is testing a new subcutaneous, or under-the-skin, formulation of Sarclisa in Phase 2 (NCT05704049) and Phase 3 trials (NCT05405166) in people with myeloma.
Common side effects of Sarclisa
The most common side effects reported for Sarclisa in clinical trials varied depending on the indication for which it was used. When used in combination with Pomalyst and dexamethasone, common side effects included:
- upper respiratory tract infections
- infusion-related reactions
- pneumonia, a potentially serious lung infection
- diarrhea
- lower counts of several types of blood cells.
When Sarclisa was used alongside Kyprolis and dexamethasone, the most common side effects included:
- upper respiratory tract infections
- infusion-related reactions
- fatigue
- high blood pressure
- diarrhea
- pneumonia
- shortness of breath
- insomnia
- bronchitis, or inflammation in the tubes that carry air to and from the lungs
- cough
- back pain
- lower counts of several types of blood cells.
Finally, the most common side effects reported in newly diagnosed patients who received Sarclisa in combination with bortezomib, lenalidomide, and dexamethasone included:
- upper respiratory tract infections
- diarrhea
- fatigue
- abnormal sensations related to nerve damage
- pneumonia
- musculoskeletal pain, or pain affecting the bones, joints, ligaments, tendons, and muscles
- cataracts, or a cloudy area in the lens of the eye
- constipation
- swelling in the arms and legs
- rash
- infusion-related reactions
- insomnia
- COVID-19
- lower counts of several types of blood cells.
Heart failure has been reported in some patients treated with Sarclisa in combination with Kyprolis and dexamethasone. Patients should be aware of this risk and immediately inform their healthcare provider if they experience potential signs of heart failure, including breathing problems, cough, or leg swelling.
Infusion-related reactions
Sarclisa treatment may result in infusion-related reactions that can be serious or life-threatening. These reactions have been mainly reported during the first infusion, and severe symptoms may include sudden stop in heart beating, abnormal blood pressure, wheezing, shortness of breath, and swelling of the face, mouth, throat, or tongue.
To reduce the risk and severity of infusion reactions, patients should be premedicated with dexamethasone, acetaminophen, and antihistamines before each Sarclisa dose. They also should be monitored for signs and symptoms of infusion-related reactions during the infusion.
If a reaction occurs, the infusion may be slowed or paused, and appropriate supportive care may be given. If paused, the infusion may be resumed at a slower rate once symptoms resolve, unless the reaction was life-threatening, in which case treatment should be permanently discontinued.
Infections
Because of its immunosuppressive effects, Sarclisa can increase the risk of severe, life-threatening, or fatal infections. Patients should be monitored for signs of infection before and during Sarclisa treatment, and receive preventive antimicrobial medications according to current guidelines.
Low immune cell counts
Sarclisa may commonly cause neutropenia, or abnormally low counts of a type of immune cell called neutrophils. Complete blood cell counts should thus be monitored regularly during treatment.
If neutropenia develops, patients should be given supportive care based on current guidelines, and be monitored for potential signs of infection. Based on neutropenia severity, Sarclisa dosing may need to be delayed until neutrophil levels recover.
New cancers
There have been reports of new cancers being diagnosed in multiple myeloma patients during and after treatment with Sarclisa-containing regimens. In Sarclisa clinical trials, the most commonly reported new cancers included skin cancers and other solid tumors. Patients should be monitored for this potential complication.
Interference in blood tests
Sarclisa can affect the results of certain blood tests, including those meant to determine compatibility between donor and recipient blood groups and to monitor treatment responses based on levels of the myeloma-associated M protein.
Because the therapy can bind to the CD38 protein at the surface of red blood cells, patients on Sarclisa may also have a false positive result on the indirect Coombs test, which assesses the presence of antibodies bound to red blood cells.
Use in pregnancy and breastfeeding
Sarclisa has not been rigorously studied in people who are pregnant, but its mechanism of action and data from animal models strongly indicate the therapy may cause fetal harm when administered during pregnancy. Specifically, Sarclisa may promote the death of fetal CD38-positive immune cells and reduce bone density.
Patients with reproductive potential should be informed about this risk, and advised to use effective forms of contraception during Sarclisa treatment and for five months after the last dose.
Pregnant women should not receive the combination of Sarclisa with Pomalyst or lenalidomide, as these medications may cause birth defects and death of the unborn child.
It remains unclear whether Sarclisa can be found in human breast milk — though similar molecules are usually present in breast milk — and whether it affects milk production or the nursing infant. Due to the potential risk of serious adverse reactions in the breastfed infant, the FDA advises against breastfeeding while taking Sarclisa.
Myeloma Research News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New targeted therapy for childhood brain cancer nears European approval
- New trial data show alnodesertib may slow ovarian cancer progression
- IMF launches Myeloma Action Month to raise global awareness this March
- Annamycin shows encouraging early results in Phase 2/3 AML clinical trial
- Clearnote’s blood test uses AI to spot pancreatic cancer in high-risk groups
Related articles
.bio-background–white {padding-bottom:0;}.bio-background–yellow {padding-bottom:2.6em;}.bio-lead-form, {display:none;}
$(document).ready(function(){//$(“.bio-background–speech .bio-type-display–medium”).remove();
$(‘h2’).each(function() {var $this = $(this);if($this.html().replace(/\s| /g, ”).length == 0)$this.remove();});
.bio-content-modules a:not([class]), .bio-widget a:not([class]) {color: #0a617c}





