Pomalyst (pomalidomide) for multiple myeloma
What is Pomalyst for multiple myeloma?
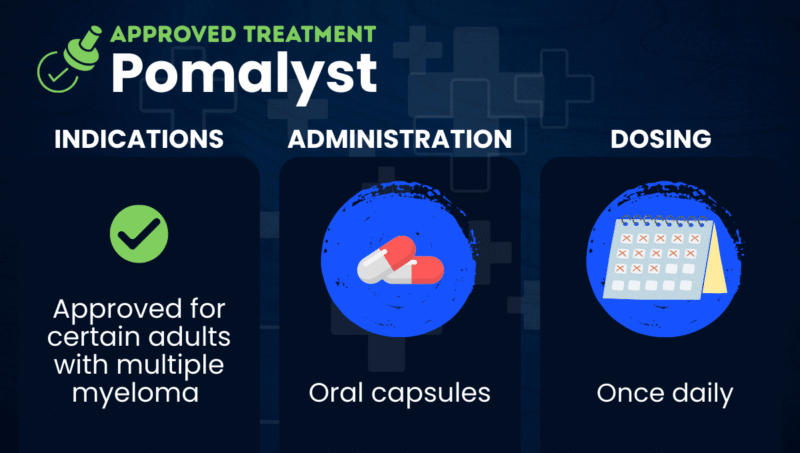
Pomalyst (pomalidomide) is an oral immunomodulatory treatment approved for certain adults with multiple myeloma when given in combination with the corticosteroid dexamethasone.
Myeloma is a type of blood cancer in which plasma cells, a type of immune cell, become cancerous and grow out of control in the bone marrow, the spongy tissue inside bones where blood cells are made.
Pomalyst works in several ways to inhibit the growth and survival of myeloma cells. It helps destroy cancer cells by breaking down proteins they need to survive. It also affects the immune system, helping immune cells better recognize and attack cancer cells while reducing signals that support tumor growth. In addition, Pomalyst can limit the blood supply that supports myeloma cell growth in the bone marrow.
Pomalyst is similar to Revlimid (lenalidomide) and Thalomid (thalidomide), which are also immunomodulatory therapies. However, each medication works slightly differently and has its own side effect profile.
Pomalyst was originally developed by Celgene, which was later acquired by Bristol Myers Squibb, the company that now markets the therapy. Generics are also available.
In addition to multiple myeloma, Pomalyst is also approved to treat AIDS-related Kaposi sarcoma, a cancer caused by viral infection.
Therapy snapshot
| Brand name | Pomalyst |
| Chemical name | Pomalidomide |
| Usage | Used to treat certain adults with multiple myeloma |
| Administration | Oral capsules |
Who with multiple myeloma can take Pomalyst?
In the U.S., Pomalyst is approved for adults with multiple myeloma when used together with dexamethasone. It is intended for people who have already received at least two prior therapies, including Revlimid and a proteasome inhibitor, and whose disease worsened during or within 60 days after their most recent therapy.
Pomalyst is contraindicated, meaning it should not be used, during pregnancy or in people who have had severe immune reactions to the therapy or its ingredients.
Pomalyst carries a boxed warning that it may cause severe birth defects or fetal death. Because of this risk, the medication is available in the U.S. only through a restricted distribution program called PS-Pomalidomide Risk Evaluation and Mitigation Strategy (REMS).
The boxed warning also notes that patients taking Pomalyst may experience a range of blood-clotting events. Doctors may prescribe medications to help reduce this risk while patients are taking Pomalyst.
How is Pomalyst administered in multiple myeloma?
Pomalyst is available as capsules that can be taken at home, with or without food. Capsules should be swallowed whole with water and should not be opened, broken, or chewed.
The recommended dosage is 4 mg once daily for 21 days out of a 28-day cycle. Treatment usually continues until disease progression. The recommended daily dose may be lower for patients with kidney or liver function impairments.
Females who can become pregnant must have two negative pregnancy tests before starting treatment.
Pomalyst in multiple myeloma clinical trials
Two clinical trials supported the approval of Pomalyst in the U.S. as a combination therapy with dexamethasone for multiple myeloma. Both studies included patients previously treated with Revlimid and the proteasome inhibitor Velcade (bortezomib).
- In a Phase 2 trial (NCT00833833), participants received either Pomalyst alone or Pomalyst plus a low dose of dexamethasone. Results showed that combining Pomalyst with dexamethasone led to better treatment responses than using Pomalyst alone.
- The Phase 3 NIMBUS trial (NCT01311687) tested Pomalyst plus low-dose dexamethasone against high-dose dexamethasone alone. Data showed the Pomalyst combination reduced the risk of disease progression or death.
Pomalyst side effects
The most common side effects of Pomalyst include:
- fatigue and weakness
- low blood cell counts
- constipation
- nausea
- diarrhea
- shortness of breath
- upper respiratory tract infections
- back pain
- fever
The prescribing information for Pomalyst also includes warnings for other potentially serious side effects, including:
- severely low blood cell counts, especially very low neutrophil counts (neutropenia)
- liver toxicity
- severe skin reactions
- tumor lysis syndrome, a serious condition that can occur when many cancer cells die quickly, particularly in people with a high disease burden
- allergic reactions, including swelling and a severe reaction called anaphylaxis
If severe skin or allergic reactions occur, Pomalyst should be permanently stopped. Patients should also be monitored for signs of neutropenia or liver toxicity, which may require pausing treatment or dose adjustments.
Blood clotting problems, including deep vein thrombosis and stroke, have been reported in people with multiple myeloma taking Pomalyst. Doctors may prescribe medications to help prevent blood clots while patients are receiving treatment.
Pomalyst must not be used during pregnancy because it can cause severe birth defects or fetal death. Females who can become pregnant must avoid pregnancy for at least four weeks before starting treatment, during treatment, and for at least four weeks after stopping treatment. During this time, they must either avoid sexual intercourse or use two reliable forms of birth control.
Because Pomalyst can be present in semen, males of reproductive potential taking the medication must use effective contraception during sexual activity with a partner who can become pregnant while taking Pomalyst and for at least four weeks after stopping treatment. They should not donate sperm during this time.
Patients should not donate blood while taking Pomalyst and for at least four weeks after stopping treatment. This helps prevent exposing a pregnant woman to the medication through donated blood.
Adding the cancer antibody therapy Keytruda (pembrolizumab) to dexamethasone and medications like Pomalyst, which are structurally similar to Thalomid, may increase the risk of mortality.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by