Protein Identified that May Point to Myeloma Patients Likely to Respond to Proteasome Inhibitors
Written by |
Researchers at The University of Texas MD Anderson Cancer Center, in collaboration with other institutions, identified a gene called TJP1 that could help predict which multiple myeloma (MM) patients are most likely to respond and benefit from proteasome inhibitor drugs like bortezomib.
The findings, “Tight Junction Protein 1 Modulates Proteasome Capacity and Proteasome Inhibitor Sensitivity in Multiple Myeloma via EGFR/JAK1/STAT3 Signaling,” were published in Cancer Cell.
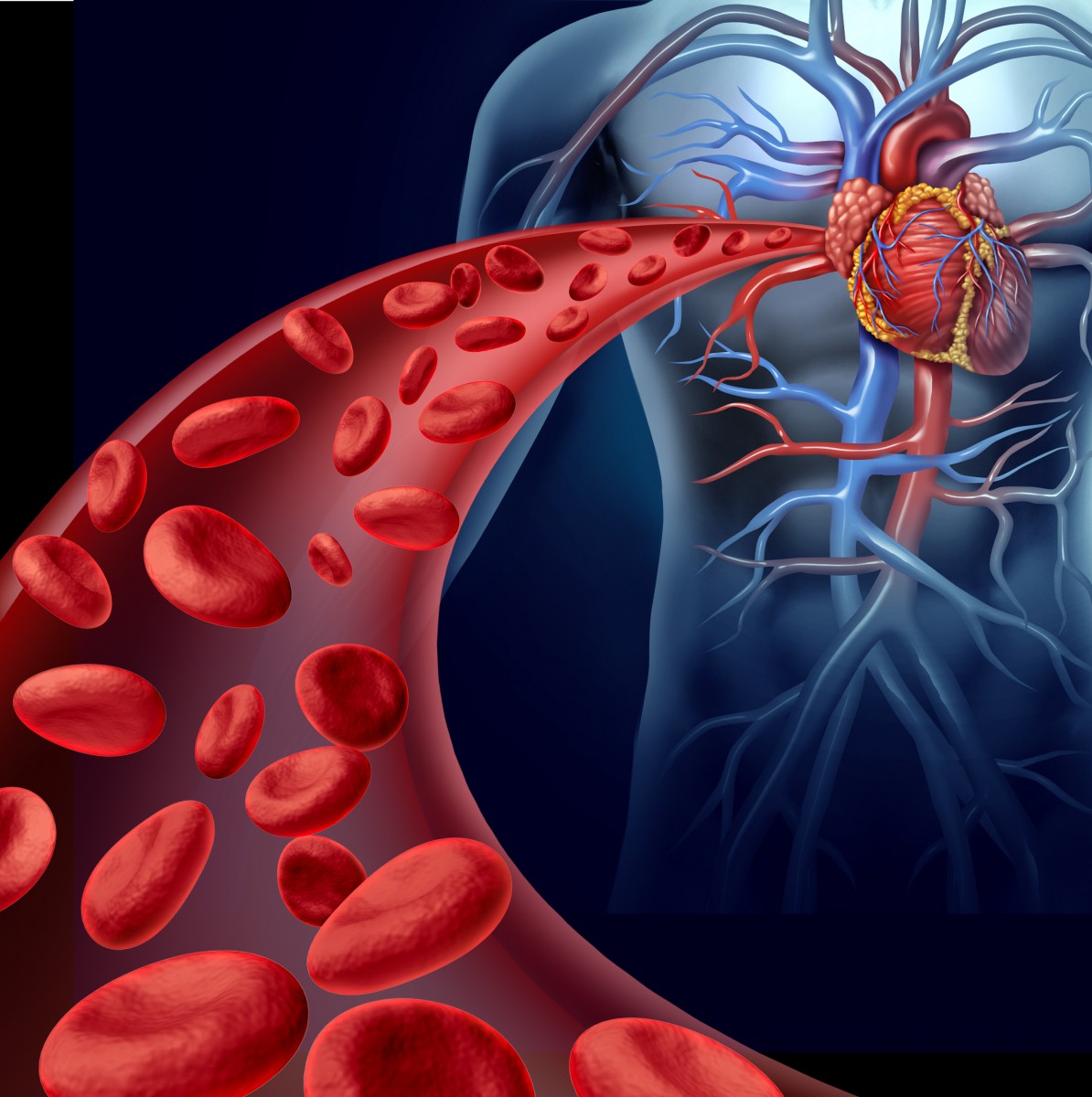
Multiple myeloma, often called myloma, is the second most common form of blood cancer, characterized by the accumulation of abnormal plasma cells in the bone marrow that interferes with the production of normal blood cells. The most common therapeutic approach for myeloma are proteasome inhibitor drugs such as bortezomib.
In some cancers like myeloma, the proteins that usually fight and kill the cancer cells are broken down at accelerated rates. Drugs like bortezomib are designed to interrupt the process and allow those proteins to maintain their function in fighting tumor cells.
“Proteasome inhibitors form the cornerstone of our standard therapy for multiple myeloma. However, no biomarkers have been clinically validated that can identify patients most likely to respond to this treatment,” said study lead Robert Orlowski, M.D., Ph.D., chair ad interim of Lymphoma/Myeloma, in the press release. “Our findings provide a rationale for the use of TJP1 as the first biomarker to select patients who are most and least likely to benefit from proteasome inhibitors.”
Researchers identified the gene TJP1, which encodes a molecule called tight junction protein 1 involved in signaling at cell-cell junctions, as a determinant of cell proteasome inhibitor sensitivity. They demonstrated that TJP1 eliminates the expression of proteins called LMP7 and LMP2. It also reduces the activity of the protein complexes and increases their sensitivity to inhibitors in both in vitro and in vivo models.
In this process, TJP1 plays the role of a mediator to suppress the signaling in protein complexes called EGFR/JAK1/STAT3, responsible for adjusting levels of the proteins LMP7 and LMP2.
“Therefore, these plasma cells were resistant to proteasome inhibitors,” Orlowski said. “Moreover, they demonstrated a previously unknown role for EGFR signaling in myeloma, and for STAT3 in controlling the level of proteasomes in cells, and therefore the cell’s ability to break down proteins.”
The researchers also found that elevated expression of TJP1 in myeloma patients is clinically linked to higher responses to bortezomib and extended response duration. By contrast, patients with myeloma cells expressing low levels TJP1 are unlikely to benefit from bortezomib.
“This study allows us to identify promising future directions to overcome proteasome inhibitor resistance in patients with high signaling through EGFR/JAK1/STAT3 pathway by offering combination therapies such as bortezomib with either the EGFR inhibitor erlotinib, or a JAK1 inhibitor such as ruxolitinib,” Orlowski said.