MS Therapy May Ease Painful Side Effect of Velcade Treatment in Myeloma Patients, Study Says
Written by |
A multiple sclerosis (MS) treatment reduced a common painful side effect of Velcade (bortezomib) in a mouse model, suggesting that it might help myeloma patients complete their treatment and ease the persistent pain of myeloma survivors.
Findings were published in the Journal of Experimental Medicine, in the study, “Dysregulation of sphingolipid metabolism contributes to bortezomib-induced neuropathic pain.”
Chemotherapy-induced peripheral neuropathy (CIPN) is a common adverse effect of several widely used cancer therapeutics, including Velcade — a treatment for multiple myeloma and mantle cell lymphoma, which causes CIPN in more than 40 percent of patients.
Peripheral neuropathy — a disabling condition that develops after damage to the peripheral nerves — often causes weakness, numbness, and pain, usually in the hands and feet.
Severe CIPN may require dose reduction or discontinuation of the treatment altogether, and even then around 30 percent of patients will continue to have symptoms, which impairs their daily activities and quality of life. Currently, no effective strategies to prevent or reduce CIPN are available.
“This growing problem is a major unmet clinical need because the increased efficacy of cancer therapy has resulted in nearly 14 million cancer survivors in the United States, many suffering from the long-term side effects of CIPN,” Daniela Salvemini, PhD, the study’s senior author and a professor of pharmacology and physiology at the Saint Louis University School of Medicine, said in a press release.
The mechanisms behind CIPN identified so far are diverse, but much of the research has focused on alterations in nerve cells, since changes in the communication processes between these cells have been implicated in CIPN.
Alterations in a type of fat molecule called sphingolipids have been associated with chronic neuropathic pain and neurodegenerative diseases, such as MS. Sphingolipids are involved in nerve cell function and communication, and were shown to regulate astrocytes — non-nerve cells that provide both metabolic (nutrients) and physical support to nerve cells.
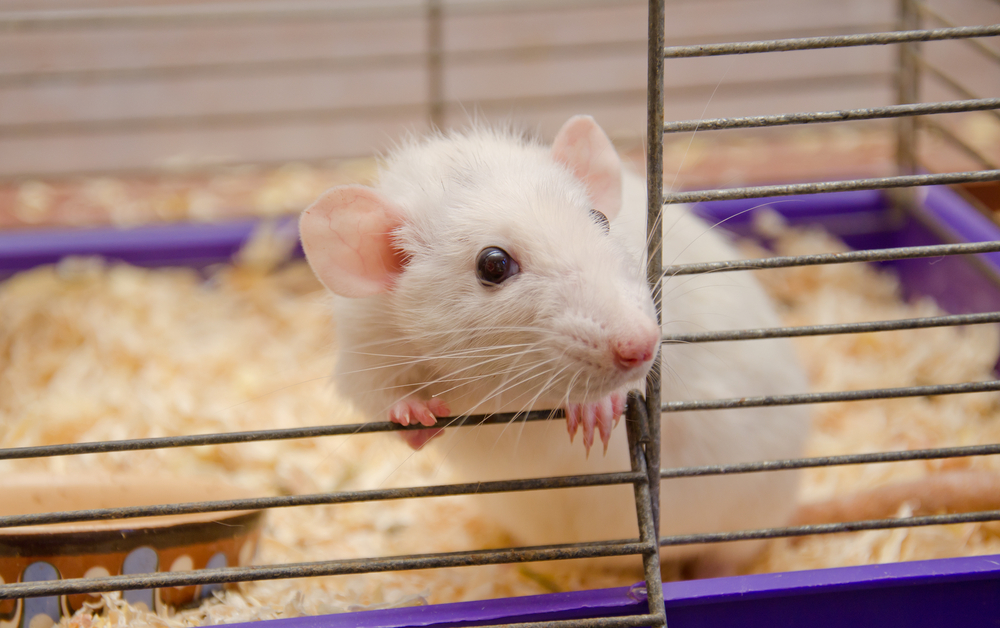
To investigate the mechanisms behind Velcade-associated peripheral neuropathy, researchers at Saint Louis University School of Medicine analyzed the nerve cells of rats treated with Velcade.
Velcade treatment led to the production and accumulation of two sphingosine molecules that bind to sphingosine-1-phosphate receptor 1 (S1PR1) — sphingosine 1-phosphate and dihydrosphingosine 1-phosphate — in the spinal cord of rats, when signs of neuropathic pain started to appear.
These effects were found to be caused by the activation of astrocytes through S1PR1, which resulted in nerve cell inflammation and an increase in the release of glutamate — a chemical messenger — from nerve cells.
Genetically deleting S1PR1 or blocking it with several therapies prevented the development of CIPN in these rats.
“Our findings establish S1PR1 as a target for therapeutic intervention and provide insight into cellular and molecular pathways,” the researchers wrote in the study.
One of the suppressive treatments used in the study was Gilenya (fingolimod), an FDA-approved MS treatment, marketed by Novartis. Gilenya binds to S1PR1 with a strength higher than sphingosine 1-phosphate, blocking the receptor’s function.
Researchers also found that Gilenya did not interfere with Velcade’s ability to kill myeloma cells, and in fact, it has been reported to possess anti-cancer properties and to enhance the effects of Velcade.
“Because fingolimod [Gilenya] shows promising anticancer potential and is already FDA approved, we think that our findings in rats can be rapidly translated to the clinic to prevent and treat bortezomib-induced neuropathic pain,” Salvemini said in the release.