Gynecological cancer overview
Last updated Dec. 18, 2024, by Lindsey Shapiro, PhD

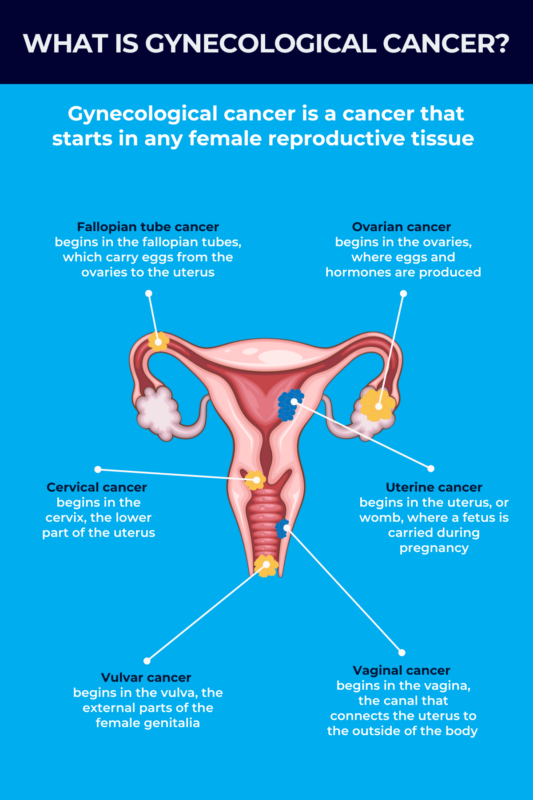
Gynecological cancer encompasses a group of cancers affecting the female reproductive system. Approximately 100,000 people are diagnosed with gynecological cancer in the U.S. every year.
Although each type of gynecological cancer is unique, with its own symptoms, risk factors, and treatment options, reaching an early diagnosis is critical for ensuring the best possible outcomes in any of them.
All individuals thus are encouraged to report to their doctor if they experience a gynecologic change that’s not normal for their body, and to meet with a gynecologist annually, even if nothing is wrong. This can help identify and address problems early on.
Types of gynecological cancers
Gynecological cancer encompasses any cancer that begins in the female reproductive system. As with other cancer types, it arises due to mutations in the DNA of cells in the affected tissue that allow cells to grow uncontrollably.
There are five main types of gynecological cancer:
- uterine cancer
- ovarian cancer
- cervical cancer
- vaginal cancer
- vulvar cancer.
While all types of gynecological cancer affect the female reproductive organs, each has its own signs and symptoms, risk factors, and treatments. Gynecological cancer life expectancy also varies by disease type and stage, among other factors.
Uterine cancer
Uterine cancer starts in the uterus, or womb, the pear-shaped organ in the female pelvis where a fetus grows during pregnancy. The most common gynecological cancer is a type of uterine cancer that affects the cells in the uterine lining, or endometrium. This form of cancer, called endometrial cancer, is often slow growing, with a good prognosis if caught early on.
Rarely, uterine cancer may form in the muscles or other supportive tissues of the uterus, and this is known as uterine sarcoma. This form is generally more aggressive than endometrial cancers.
Ovarian cancer
Ovarian cancer originates in the ovaries, which are the female reproductive organs responsible for producing eggs and hormones. This type of cancer is the second most common type of gynecological cancer. The most common form is epithelial ovarian cancer, which affects the cells lining the outside of the ovaries.
About three-quarters of epithelial ovarian cancers are called high-grade serous ovarian carcinomas, which grow slowly at first but ultimately become very aggressive. By the time they’re diagnosed, most people with this type of ovarian cancer have advanced disease that has spread outside the ovaries.
There are also other rare ovarian cancers, including mucinous ovarian cancer and ovarian sarcoma, that each affect different cells in the ovaries and have distinct outlooks.
Cervical cancer
Cervical cancer starts in the cervix, the lower part of the uterus that dilates to allow passage of the fetus during childbirth. It is the only gynecological cancer in which most cases have a known cause — specifically, infection with the human papillomavirus (HPV) — and can be detected in their early stages with a reliable screening test.
This cancer usually develops slowly over many years. If caught early, cervical cancer is considered highly treatable.
Vaginal and vulvar cancer
Vaginal and vulvar cancers begin, respectively, in the vagina — the muscular tube connecting the uterus to the outside of the body — and the vulva, referring to all external parts of the female genitalia. They are very rare, together accounting for about 7% of all gynecological cancer cases in the U.S. As with other forms of gynecological cancer, most of these cancers grow slowly over several years, and are treatable in their early stages.
Other types
A sixth type of gynecological cancer is fallopian tube cancer, which begins in the tubes that carry eggs from the ovaries to the uterus. It is often treated by medical experts like a type of ovarian cancer. Much like ovarian cancer, fallopian tube cancer often does not have symptoms early on and spreads quickly. Still, it is curable if caught and treated early.
Recent findings suggest that epithelial ovarian cancer probably originates in the fallopian tubes and then spreads to the ovaries and other pelvic and abdominal regions.
Another cancer related to ovarian cancer is primary peritoneal carcinoma, which starts in the tissue lining the abdominal cavity, or the peritoneum. Although this is not distinctly a female reproductive organ, the cells in the peritoneum are the same as the ones that are affected in epithelial ovarian cancer. Thus, they are generally treated in the same way.
Gestational trophoblastic disease refers to a very rare group of tumors that form in the uterus after conception. While they’re usually benign, or noncancerous, some can become malignant. These cancers are highly treatable, and nearly all affected people are cured.
Symptoms
Early on, gynecological cancers often do not cause any symptoms. When they do, the symptoms can vary substantially based on the individual and the cancer type.
Some possible gynecological cancer symptoms include:
- abnormal vaginal bleeding or discharge, including heavier than normal periods, bleeding in between periods, bleeding after sex, or bleeding past menopause onset, or any other type of bleeding/discharge that a person does not normally experience (all types except vulvar cancer)
- pelvic pressure or pain (uterine, ovarian, and vaginal cancers)
- pain or discomfort during sex (uterine, cervical, vaginal, and vulvar cancers)
- changes in bathroom habits, including more frequent/urgent need to urinate or constipation (ovarian, vaginal cancers)
- bloating (ovarian cancer)
- abdominal or back pain (ovarian cancer)
- feeling full too quickly or having difficulty eating (ovarian cancer)
- itching, burning, pain, or bleeding on the vulva (vulvar cancer)
- changes to the vulva’s color or skin, such as rashes, sores, or warts (vulvar cancer).
Every person’s body is different, and what is abnormal for one might not be so for another. All individuals need to pay attention to their bodies and know what’s normal for them, so it is easier to identify if something has changed.
People should talk to a doctor if they experience any vaginal bleeding that’s abnormal, or if other symptoms have persisted for more than two weeks. Many of the symptoms of gynecological cancers overlap with other noncancerous conditions. The only way to get an accurate diagnosis is to let a doctor know as soon as anything seems different.
Causes and risk factors
All individuals with female reproductive organs are at risk of gynecologic cancer, and that risk generally increases with age. Other gynecological cancer causes and risk factors vary by cancer type.
For example, nearly all cases of cervical cancer are caused by HPV, a common sexually transmitted infection (STI), as are some cases of vaginal and vulvar cancer. For most people, HPV never causes problems and clears up on its own, but certain strains of the virus can cause changes in cells that lead to cancer.
Other factors can also raise a person’s risk of cervical cancer. Often, this is because they increase the risk of HPV infection or make it less likely that the body will clear up the infection on its own. Cervical cancer risk factors include:
- smoking
- having more sexual partners, early sexual activity, or unprotected sex
- having a weakened immune system due to other health conditions
- exposure in the womb to diethylstilbestrol (DES), a synthetic form of estrogen given to pregnant people between 1940 and 1971 to prevent miscarriage.
For all other types of gynecological cancer, there is usually not a known cause. But there are certain gynecological cancer risk factors that can increase the chances a person will develop one of these conditions.
Uterine cancer risk factors include:
- obesity
- diabetes
- increased exposure to the female sex hormone estrogen
- a past history of breast or ovarian cancer
- endometrial hyperplasia, or an abnormal thickening of the uterine lining
- never having been pregnant
- exposure to tamoxifen, a hormone therapy used to treat breast cancer
- prior radiation therapy to the pelvis
- having a family history of uterine, colon, or ovarian cancer, or of Lynch syndrome, a genetic condition that increases the risk of several cancers.
A risk factor, increased estrogen exposure can come from more years of menstruation, the use of estrogen-only hormone replacement therapy during menopause, or other conditions that affect hormones, such as polycystic ovarian syndrome.
Ovarian cancer risk factors include:
- being obese or overweight
- a family history of ovarian cancer
- genetic changes linked to ovarian cancer risk, including BRCA1 or BRCA2 gene mutations and Lynch syndrome
- increased estrogen exposure
- never having been pregnant
- endometriosis, a condition in which tissue similar to the endometrium grows outside the uterus.
Vaginal cancer risk factors include:
- HPV infection
- smoking
- DES exposure.
Vulvar cancer risk factors include:
- HPV infection
- smoking
- having a weakened immune system
- a history of precancerous conditions or skin conditions affecting the vulva.
Diagnosis
Reaching an early gynecological cancer diagnosis is critical for ensuring optimal treatment outcomes in all forms of gynecological cancer. Individuals should go to the doctor as soon as they notice something unusual.
A physician will first ask about symptoms and risk factors, and collect a thorough medical and family history. There are then a series of tests the clinician might perform to identify whether or not there’s a problem.
Physical exam
The first step toward a diagnosis is usually a physical exam. This will likely involve a pelvic exam, during which a doctor examines both external and internal parts of the reproductive system. A patient will lie back on a table and bend the legs at the knees. The doctor may then:
- visually examine the vulva for any unusual changes
- insert an instrument called a speculum into the vagina to allow viewing of the vagina and cervix
- insert one or two fingers into the vagina while pressing on the abdomen, to feel for any unusual changes in the ovaries or uterus
- insert a finger into the rectum to check for lumps or abnormalities behind the uterus.
There aren’t always early signs of gynecological cancer, so routine pelvic exams, even in the absence of symptoms, may be recommended for some individuals based on their personal and family history.
During a routine pelvic exam, physicians may also perform a cervical cancer screening test called a Pap smear, in which cells are scraped from the surface of the cervix and sent to a lab to determine if they are cancerous or precancerous, meaning they have the potential to become cancerous later. The cells can also be tested for HPV. Many cervical cancer diagnoses are reached after a routine Pap smear comes back as abnormal.
Other tests
If gynecological cancer is suspected, a physician may run a series of other tests to establish if cancer is present, and if so, whether it has spread to lymph nodes or other organs. These may include:
- blood tests to look for disease-related biomarkers and check for general organ function
- an ultrasound to visualize the ovaries, uterus, or the inside of the vagina
- other imaging tests, such as CT and MRI scans, to visualize any tumors and, if found, determine their size and whether they’ve spread to other parts of the body
- tissue biopsy, in which a sample of abnormal tissue is collected and examined for signs of being cancerous.
A biopsy is the most definitive way to confirm that any abnormal tissue actually is cancer. There are several different ways a biopsy may be collected, and the procedure may sometimes involve surgery.
Depending on the cancer type, a doctor might also perform various scope procedures — where a tube with a camera attached is inserted into the body — to get a closer look at the affected tissue or to examine nearby organs. Examples include:
- a colposcopy, to look at the vulva, vagina, and cervix
- a hysteroscopy, to look at the uterus
- a cystoscopy, to see if the cancer has spread to the bladder
- a proctoscopy, to see if there are signs of cancer spreading to the small intestine or the rectum.
Treatment options
Treatment for gynecological cancer depends on the type of cancer a person has and how far it has spread. In most cases, patients receive more than one kind of treatment.
Physicians called gynecologic oncologists specialize in these forms of cancer and can help patients decide the best treatment plan for their particular case. Before making any treatment decision, patients should always talk carefully with their doctors about their treatment options and the benefits and risks of each possible approach; patients may wish to get an opinion from more than one clinician.
Gynecological cancer treatment may involve:
- surgery, to remove the cancer and other affected or at-risk tissues
- chemotherapy, where medications kill cancer cells to shrink or slow the progression of cancer
- radiation therapy, in which targeted beams of radiation are used to kill cancer cells
- targeted therapies, or medications that target specific changes in cancer cells that help them grow
- immunotherapy, or treatments that boost the immune system’s ability to fight cancer
- hormone therapy, or medications that modulate hormone levels or activity to slow cancer growth.
In general, surgery is the main treatment approach for most gynecological cancers. However, surgery might not always be possible, such as in cases in which the cancer has already spread extensively or a person is not healthy enough for the procedure.
It’s not unusual for patients to receive multiple treatment types at once or over time, depending on their situation and how well they’re responding to or tolerating specific treatment approaches.
Cancer treatment, especially chemotherapy, can cause a wide range of side effects. Supportive care measures can help manage chemotherapy side effects and maximize quality of life for patients at any stage of the disease. For people diagnosed with terminal cancer, supportive care will help them feel as comfortable as possible in their remaining months or years.
Many gynecological cancer treatments are likely to affect fertility. Before starting treatment, patients should talk with their physicians about the likelihood of their fertility being impacted and discuss potential options for fertility preservation.
Prevention and early detection
Any person with female reproductive organs can be affected by gynecological cancers, and there is no guaranteed approach for gynecological cancer prevention.
Avoiding HPV infection is the best way to prevent cervical cancer, and may also help prevent some vaginal and vulvar cancers. Several strategies may help individuals to best protect themselves:
- Practicing safe sex and always using condoms is recommended for all people.
- Getting the HPV vaccine, which protects against strains of the virus most likely to cause cancer, is recommended for all people ages 11-26, as well as some older people.
Certain modifiable factors, such as smoking and obesity, increase a person’s risk of gynecological cancers. Thus, living a healthy lifestyle — including maintaining a healthy weight, eating a well-balanced diet, exercising, and avoiding smoking and other toxic substances — can also help lower disease risk.
While preventing gynecological cancer is not possible, early detection is critical. It’s recommended that all people with female reproductive organs meet with a gynecologist to discuss their health annually. This won’t always involve a full pelvic exam, but a gynecologist might decide on annual exams depending on the person’s risk of gynecological cancer.
Routine Pap smears to screen for cervical cancer are recommended for people with a cervix starting at age 21. If tests are normal, Pap smears are usually done every three to five years until age 65.
There are no reliable screening tests for any other types of gynecological cancer. That’s why it’s especially important for individuals to monitor their bodies closely and promptly report any unusual changes or symptoms to their doctor.
Living with gynecological cancer
Living with gynecological cancer can take a significant physical and emotional toll on a patient. After being diagnosed, there are a few things a person can do to help ease stress and live as well as possible:
- Stay informed about gynecological cancer, treatment options, and available clinical studies. This can help patients feel more empowered and enable them to make the best possible decisions for themselves.
- Communicate with healthcare providers about symptoms, side effects, and any other concerns. Making sure doctors know exactly how cancer, and treatment, are affecting patients will help them get the best possible care.
- Monitor mental health and emotional well-being. Patients should check in with themselves about how they’re feeling and find strategies to help themselves cope with stress.
- Make necessary lifestyle changes. Patients might find that they need to change their daily routine to adjust for the symptoms and side effects that come with gynecological cancer and its treatment.
- Build a good support system. Getting through gynecological cancer treatment is hard. Patients should let their caregivers, friends, family, and other members of their support system know what they need to make it easier.
A number of resources are available to support people living with gynecological cancer. The Society of Gynecologic Cancer offers a list of such resources for patients and families, with information about specific cancers, support groups, and clinical trials.
Rare Cancer News can also serve as a resource for individuals affected by gynecological cancers, such as patients, their caregivers, and their loved ones. It provides up-to-date information on research advancements and treatment options, as well as educational materials for those who may want to know more about the condition.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Clearnote’s blood test uses AI to spot pancreatic cancer in high-risk groups
- Being a caregiver requires constant, sometimes impossible, calculations
- Immuno-gene therapy for brain cancer tumors now on FDA fast track
- FDA approves Keytruda for hard-to-treat gynecological cancers
- FDA reviewing new iberdomide combo for hard-to-treat multiple myeloma
Related articles