Elrexfio (elranatamab-bcmm) for multiple myeloma
Last updated Aug. 27, 2024, by Marta Figueiredo, PhD

What is Elrexfio for multiple myeloma?
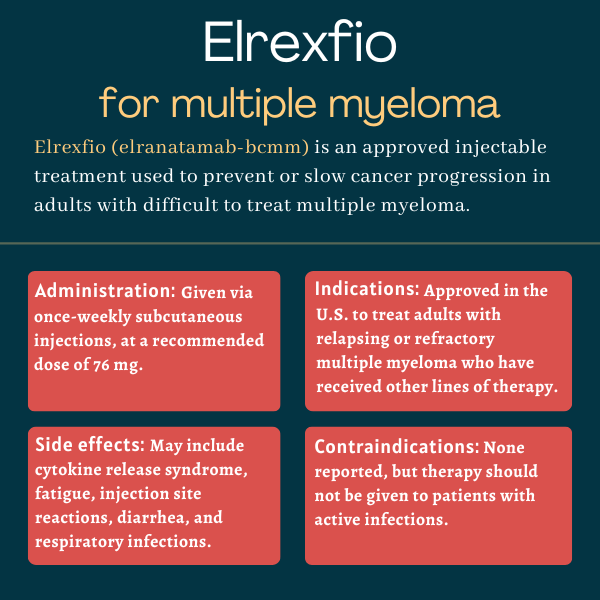
Elrexfio (elranatamab-bcmm) is an under-the-skin, or subcutaneous, injectable therapy approved in the U.S. for adults with relapsed or refractory multiple myeloma (RRMM) who have received at least four previous lines of treatment.
The therapy, developed by Pfizer, is expected to help bring cancer under control or slow its progression by bringing together cancer-fighting immune T-cells and myeloma cells.
The medication is conditionally approved in the U.S. and other regions based on early evidence that it results in clinically meaningful, long-lasting responses in which the cancer does not show signs of progression. Additional clinical trial data confirming Elrexfio’s clinical benefit in this patient population will be needed for full regulatory approval.
Therapy snapshot
| Brand name: | Elrexfio |
| Chemical name: | Elranatamab-bcmm |
| Usage: | Used as a late line of therapy for adults with hard-to-treat multiple myeloma; may help slow cancer progression |
| Administration: | Subcutaneous injection |
How does Elrexfio work?
Multiple myeloma is a rare blood cancer that starts in the bone marrow, where blood cells are formed, and can spread throughout the body.
It is characterized by uncontrolled growth of plasma cells, the type of immune cell responsible for producing high levels of antibodies that normally help the body fight infections and other threats. Cancerous plasma cells, called myeloma cells, instead produce an abnormal antibody, called M protein, that can cause complications.
The rapid buildup of myeloma cells, which limits the natural growth of other types of blood cells in the bone marrow, as well as the M protein, can cause a range of disease symptoms, including bone damage, blood abnormalities, kidney problems, and nerve system issues.
While many treatment options are available for multiple myeloma, the cancer can nonetheless be difficult to treat because it is often refractory, meaning it does not respond to such therapies, or has relapsed, meaning it comes back after treatment helps achieve disease remission.
Elrexfio, formerly known as PF-06863135, is a bispecific antibody, meaning it can interact with two different targets at the same time. It’s designed to simultaneously bind to B-cell maturation antigen, or BCMA, a protein found at high levels at the surface of myeloma cells, and the CD3 protein on the surface of immune T-cells, which have natural cancer-fighting abilities.
The medication serves as a bridge between these two cell types, guiding T-cells to BCMA-positive myeloma cells, and subsequently triggering a cancer-killing immune attack. As such, Elrexfio is expected to help eliminate myeloma cells, keeping cancer under control and slowing or halting its progression.
Who can take Elrexfio?
Elrexfio was granted conditional approval by the U.S. Food and Drug Administration (FDA) in August 2023 to treat adults with relapsed or refractory multiple myeloma who have received at least four prior lines of treatment. These treatments include a proteasome inhibitor (PI), an immunomodulatory agent (IMiD), and a CD38 inhibitor (or anti-CD38 antibody).
Conditional, or accelerated, approval means that the therapy can be marketed based on less comprehensive safety and efficacy data than normally are required, and that additional clinical trial results confirming its benefits are needed for full approval.
The regulatory decision made Elrexfio the first BCMA-CD3-directed bispecific antibody approved in the U.S. with the possibility of dosing every other week, instead of once weekly, for certain myeloma patients. Pfizer said at the time of approval that this less-frequent dosing regimen may be more convenient for patients and be associated with a more favorable safety profile.
For individuals in the U.S. who are prescribed Elrexfio, Pfizer’s Oncology Together program is available to help provide personalized support, including help with insurance coverage navigation.
The therapy also is approved in Canada and the European Union for adults with RRMM who have previously received three or more lines of treatment. The types of included therapy lines are the same as those covered by the U.S. label.
Elrexfio can increase the risk of certain immune responses and neurologic toxicity that can be serious and life-threatening. These include cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). Therefore, the therapy in the U.S. is available only through a restricted access program called Elrexfio Risk Evaluation and Mitigation Strategy (REMS).
This program ensures that only certified healthcare professionals can prescribe Elrexfio, and that both physicians and patients are fully informed about its risks and equipped to respond effectively if any signs of treatment reactions become apparent.
Who should not take Elrexfio?
Elrexfio’s prescribing information lists no contraindications. However, patients with an active infection should not start treatment with Elrexfio.
How is Elrexfio administered in multiple myeloma?
Elrexfio is administered by a healthcare provider through subcutaneous injections, at a recommended dose of 76 mg, once a week or once every other week.
First, however, two injections, called step-up doses, are given in the first week of treatment due to the risk of CRS. Specifically, the first injection is given at a dose of 12 mg on day 1, and the second at a dose of 32 mg on day 4. Patients should be hospitalized for two days after administration of the first step-up dose, and for one day after the second step-up dose, to monitor for adverse reactions.
On day 8, patients receive their first 76 mg treatment dose. Doses are then given once weekly until week 24, which is nearly six months altogether. After 24 or more weeks of treatment, patients who achieve a partial or better response to Elrexfio and maintain such a response for at least two months should start to receive the therapy once every two weeks.
Each injection of Elrexfio, available as single-use vials, is given by a healthcare provider with adequate medical personnel and equipment at the ready to manage potential severe reactions, including CRS and ICANS. Elrexfio typically is injected into the abdominal area (stomach), in a region without tattoos, scars, or bruised, red, tender, or hard skin.
About one hour before each of the first three doses — the two step-up doses and the first 76 mg dose — patients should receive three types of premedication to help reduce the risk of cytokine release syndrome:
- an oral anti-fever medication such as acetaminophen (sold as Tylenol, among others)
- a corticosteroid, such as dexamethasone, administered either orally or directly into the bloodstream
- an oral antihistamine such as diphenhydramine.
If a planned dose of Elrexfio is missed, treatment should be resumed according to label recommendations, which vary based on the type of the last dose (step-up dose 1, 2, and treatment dose) and the time since the last dose.
Elrexfio in clinical trials
Conditional approval of Elrexfio in the U.S. was mainly supported by data from the Phase 2 MagnetisMM-3 clinical trial (NCT04649359). Full approval is pending the results of a confirmatory Phase 3 trial called MagnetisMM-5 (NCT05020236).
MagnetisMM-3
The global Phase 2 MagnetisMM-3 study was designed to evaluate the safety and efficacy of Elrexfio in adults with RRMM who had received at least three therapy lines, including a PI, an IMiD, and an anti-CD38 antibody.
The study enrolled 187 patients. After two step-up doses in the first week, all received an injection of 76 mg Elrexfio once weekly in cycles of about four weeks. Those achieving a partial response (cancer reduction) or better for at least two months after receiving six or more treatment cycles could move to an every other week dosing schedule.
The main goal was to assess response rates at about 16 months, or nearly 1.5 years. Secondary goals included time to response, duration of response, minimal residual disease (MRD) negativity, progression-free survival (PFS), overall survival, and safety measures. MRD refers to the small number of myeloma cells that may remain after treatment and cause a relapse, while PFS concerns the time a person lives without signs of disease progression.
Conditional approvals were supported by results from the group of 123 participants who had not received previous treatment with a BCMA-targeted agent.
Over a median follow-up of more than a year, 61% of patients responded to Elrexfio, with 35% achieving a complete response, or having no signs of cancer. Furthermore, most (80%) of the 50 patients who switched to every other week dosing maintained or improved their response over six months or longer after the switch.
The FDA’s clearance was specifically based on data from the 97 participants who had received four or more lines of therapy. With a median follow-up of 11 months, or nearly one year, more than half of these patients (57.7%) responded to Elrexfio, with about one-quarter experiencing a complete response.
Median response duration had not been reached, meaning that most patients were still responding to treatment. Also, 82.3% of responders were estimated to maintain such a response for at least nine months.
The trial also enrolled a group of 64 patients who had previously received BCMA-directed therapies, and all but one had been given at least four therapy lines. A median of 10.2 months of follow-up data from those 63 patients demonstrated that one-third of them responded to treatment, and 84.3% sustained a response for at least nine months.
MagnetisMM-5
The ongoing, global, two-part Phase 3 MagnetisMM-5 trial is expected to involve up to 761 adults with RRMM who have received at least one previous therapy line, including lenalidomide (sold as Revlimid and with generics available) and a proteasome inhibitor. None of the participants may have received prior treatment with a BCMA-targeted agent.
Slated to run through 2027, the study aims to test Elrexfio, alone or in combination with Darzalex Faspro (daratumumab and hyaluronidase-fihj) against the standard treatment combination of Darzalex Faspro, pomalidomide (sold as Pomalyst and generics), and dexamethasone. Darzalex Faspro is the subcutaneous formulation of Darzalex (daratumumab), an older myeloma therapy that is infused intravenously, or directly into the bloodstream.
The first part of MagnetisMM-5 is designed to test several doses of Elrexfio, when combined with Darzalex Faspro, to determine the optimal Elrexfio dose for the combination treatment. In the second part, participants are randomly assigned to receive either Elrexfio alone, the Elrexfio-Darzalex Faspro combo, or standard combination treatment.
The main goal of the trial’s second part is to compare patients’ PFS between the three treatment groups for up to about four years. Secondary goals include overall survival, response rates, response duration, time to response, rates of MRD negativity, and safety measures.
Common side effects of Elrexfio
The most commonly reported side effects with Elrexfio include:
- cytokine release syndrome
- fatigue
- an injection site reaction, such as redness, pain, itching, and/or swelling
- diarrhea
- an upper respiratory tract infection
- muscle and bone pain
- pneumonia, a serious lung infection
- reduced appetite
- rash
- cough
- nausea
- fever
- lower counts of several types of blood cells.
Cytokine release syndrome
Due to its mechanism of action, Elrexfio carries a boxed warning noting that it may lead to potentially fatal CRS, a sudden, heightened inflammatory response that can cause a wide range of symptoms, including fever, a rapid heartbeat, low blood pressure, headache, trouble breathing, and increased levels of liver enzymes, which indicates liver damage.
In MagnetisMM-3, CRS occurred in more than half of Elrexfio-treated participants, most often after the first or second step-up dose, and at a median of two days after dosing.
To reduce the risk of CRS, patients prescribed Elrexfio should follow the therapy’s recommended step-up dosing schedule, receive the recommended premedication before each step-up dose, and be carefully monitored in the days after administration.
If signs or symptoms suggestive of CRS are experienced, patients should seek immediate medical attention; if confirmed, CRS should be managed according to recommendations.
Treatment should be interrupted until cytokine release syndrome is resolved, or permanently stopped based on the severity of the reaction.
Neurologic toxicity, including ICANS
The therapy’s boxed warning also mentions the increased risk for serious or life-threatening neurologic toxicity, including immune effector cell-associated neurotoxicity syndrome.
ICANS is a serious form of brain dysfunction that can cause neurological symptoms such as confusion, mood swings, seizures, loss of coordination, an altered level of consciousness, and brain swelling.
In MagnetisMM-3, neurologic toxicity was reported in more than half of patients given Elrexfio, and ICANS in fewer than 5%. Most of these brain inflammation reactions occurred after the first step-up dose and at a median of three days after the most recent dose. The onset of ICANS may occur simultaneously with CRS, following cytokine release syndrome resolution, or in the absence of CRS.
Patients should be closely monitored for signs and symptoms of neurologic toxicity during Elrexfio treatment, and if anything is detected, patients should be immediately evaluated. Decisions regarding appropriate treatment and whether Elrexfio should be withheld or permanently discontinued should be based on severity.
Due to the risk of a reduced level of consciousness associated with neurologic toxicity, patients on Elrexfio should not drive or operate dangerous machinery for two days after receiving each of the two step-up doses and the first treatment dose. If the patient develops any neurological symptoms during treatment, these types of activities should also be avoided until such symptoms are resolved.
Infections
Because of its suppressive effects on the immune system, Elrexfio also can increase the risk of serious and fatal infections. Patients should be monitored for signs of infection before Elrexfio treatment and receive preventive antimicrobial and antiviral medications according to current guidelines.
Those with an active infection before treatment should not start Elrexfio, and those who develop an infection while on the therapy should be given appropriate medication and either interrupt or discontinue Elrexfio based on infection severity.
Low immune cell counts
Elrexfio may cause neutropenia, or abnormally low counts of a type of immune cell called neutrophils, as well as febrile neutropenia, which refers to fever during a period of neutropenia. As such, complete blood cell counts should be monitored at the therapy’s start and regularly during treatment.
Patients with neutropenia should be given supportive care based on current guidelines, and be monitored for potential infections. Based on neutropenia severity, Elrexfio may need to be interrupted.
Liver damage
Elrexfio can cause liver damage, as reflected by higher than normal blood levels of the liver enzymes alanine transaminase (ALT) and aspartate aminotransferase (AST), and the bilirubin protein. Increases in blood liver enzyme levels may occur together with or independently of CRS.
As such, patients’ liver enzymes and bilirubin should be monitored through blood tests at the start of Elrexfio therapy and during treatment as appropriate. The therapy should be withheld or permanently discontinued based on liver damage severity.
Use in pregnancy and breastfeeding
Elrexfio has not been rigorously studied in people who are pregnant or breastfeeding nor in animal reproductive or developmental studies. However, based on its ability to activate T-cells, promote the release of inflammatory and immune molecules, and reduce the number of immune B-cells, the therapy is likely to cause fetal harm when administered during pregnancy.
Patients who have the potential to become pregnant should be informed about this potential risk to a developing fetus, and advised to use effective forms of contraception while taking Elrexfio and for four months after the last dose.
A pregnancy test should be conducted before starting Elrexfio, and patients should immediately tell their doctors while on the therapy if they suspect they might be pregnant.
No data are available about whether Elrexfio is excreted in human milk, though similar molecules are usually present in breast milk. Given that it remains unknown whether this poses a risk for a nursing infant, the FDA advises against breastfeeding while taking Elrexfio and for at least four months after the last dose.
Myeloma Research News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- FDA OKs label changes to boost CAR T-cell therapy use for cancer
- Oral Inqovi, venetoclax for acute myeloid leukemia to be reviewed
- Daraxonrasib granted breakthrough designation for pancreatic cancer
- The art of distraction: Why sometimes we avoid ‘cancer talk’
- Stories being shared in honor of Glioblastoma Awareness Day
Related articles