Blood cancer overview
Last updated Jan. 6, 2025, by Marisa Wexler, MS

Blood cancer is a broad term encompassing diseases in which blood cells grow too much or develop abnormally. Typically, blood cancers are classified into three main categories – leukemia, lymphoma, and myeloma – but they can be further divided into dozens of specific types, each with unique features.
Although blood cancers can be life-threatening, there are many treatments available to manage these diseases, and most people diagnosed with blood cancer will survive for many years after the diagnosis.
What is blood cancer?
Cancers are diseases in which the body’s own cells start to grow and multiply out of control. Blood cancer, therefore, refers to cancers in which blood cells turn cancerous.
There are many different types of blood cells, including red blood cells, which carry oxygen through the body, and white blood cells, which are part of the immune system and help defend the body against infections.
All blood cells develop within the bone marrow, the soft tissue found inside bones. This unique environment contains specialized cells called hematopoietic stem cells, or HSCs. HSCs have the ability to multiply and transform into all the various blood cell types, and they maintain a continuous process of growth and division to produce a constant supply of new blood cells throughout a person’s life.
Blood cancer develops when mutations occur within the DNA of blood cells and disrupt their normal behavior. Some types of blood cancer occur when HSCs or immature blood cells in the bone marrow start to multiply out of control. Other forms of these cancers occur due to the abnormal growth of mature blood cells.
Blood cancers are classified into different types depending on the specific type of cell involved and how they grow in the body.
Three types of blood cancer
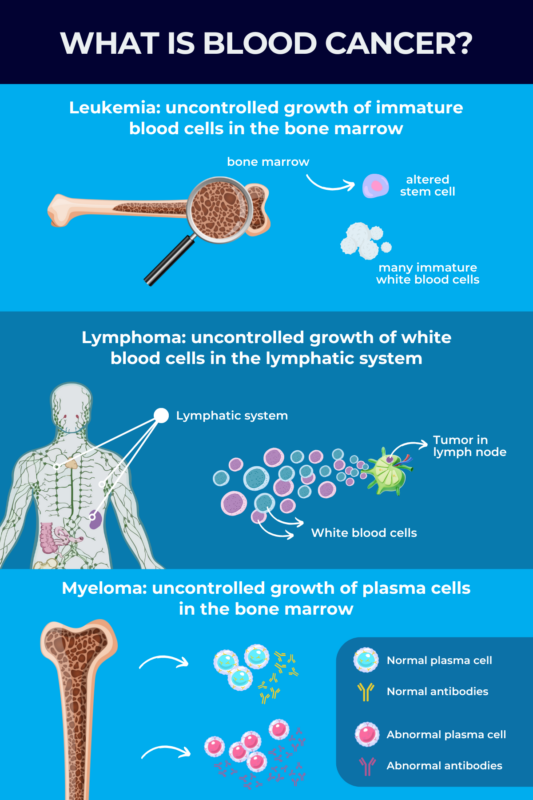
Blood cancer is commonly classified into three main types: leukemia, lymphoma, and myeloma. Within these three broad types are many subtypes, each within one of these general categories. In fact, more than 100 distinct types of blood cancer have been defined.
Leukemia
Leukemia is the most common blood cancer in the U.S., and the most common type of cancer that occurs in children. It starts in the bone marrow when immature blood cells begin to grow out of control, taking up excessive amounts of space in the bone marrow and ultimately traveling out into the bloodstream.
This disease form usually involves immature white blood cells, though other types of blood cells can also cause leukemia. Unlike most other types of cancer, leukemia does not result in solid masses or tumors — instead, leukemia cells become dispersed throughout the bloodstream.
Leukemia can be classified based on how quickly it progresses, and the type of blood cell involved. There are four main types of leukemia:
- Acute lymphocytic leukemia, or ALL, is the most prevalent leukemia type in children, teens, and young adults.
- Acute myeloid leukemia, known as AML, is the most common acute leukemia among adults; however, it can also affect children.
- Chronic lymphocytic leukemia, or CLL, is the most common chronic leukemia in adults; CLL symptoms may not manifest for several years.
- Chronic myeloid leukemia, called CML, is more prevalent in older adults and rarely occurs in children.
Lymphoma
Lymphoma is a blood cancer that affects the lymphatic system, which includes the lymph nodes. If the immune system is the body’s army, the lymph nodes are its barracks – solid organs where immune cells live when they aren’t waging battles elsewhere.
In lymphomas, white blood cells in the lymph nodes start to multiply out of control, ultimately growing into tumors in the lymphatic system. While leukemia and lymphoma both typically involve the uncontrolled growth of white blood cells, lymphoma is characterized by tumors but leukemia is not; this is generally an easy way to distinguish between the two.
There are two main types of lymphoma:
- Hodgkin lymphoma, which typically affects younger adults, ages 20 to 39, or those older than 65
- non-Hodgkin lymphoma, which typically affects older adults, ages 60 to 80.
Myeloma
Myeloma is caused by the uncontrolled proliferation of plasma cells — a type of immune cell responsible for producing infection-fighting proteins known as antibodies. Plasma cells are mature B-cells that play a critical role in the immune system.
In myeloma, abnormal plasma cells grow out of control in the bone marrow, taking up space and disrupting the normal growth of other blood cells. Myeloma is often called multiple myeloma because it typically affects multiple parts of the body; functionally, multiple myeloma is a synonym for myeloma.
Causes
Blood cancer causes are not fully understood, but all such cancers are thought to develop because of mutations in the DNA of blood cells.
A cell’s DNA is like an instruction manual that tells the cell how to behave. Mutations are changes in the genetic code that cause a cell to get the wrong instructions. As a result, cells grow when they shouldn’t, and this uncontrolled growth ultimately leads to the development of cancer.
Although mutations are thought to underlie all blood cancers, it is not clear exactly what causes such alterations to occur in the first place. In many cases, mutations may occur due to random chance when cells are growing. In other cases, certain risk factors can increase the chances of developing blood cancer.
Age
As new blood cells are constantly being produced, the risk of blood cancer tends to increase with age. The longer people live, the more blood cells have been made in their lifetime, so there are more chances for something to go wrong.
Exposure to environmental factors
The risk of developing blood cancer can also be increased by exposure to substances that are known to be able to trigger mutations; such substances are known as carcinogens. Among them are high doses of radiation, certain chemicals like herbicides, insecticides, or benzenes, and smoking cigarettes.
Medications and treatments
Many of the medications that are used to treat cancer can also trigger mutations in healthy cells. Thus, somewhat paradoxically, receiving cancer treatments may increase the risk of developing future blood cancers.
Individual risk factors
Demographics, family history, and other health conditions also can affect the risk of developing blood cancers. For example, many types of blood cancer are more common in men than in women. Myeloma is more common in people of African descent than in other racial and ethnic groups, and people who are obese are also more likely to develop this cancer type.
Immune system and viral infections
People with weakened immune systems or autoimmune conditions are more likely to develop lymphomas. Additionally, individuals with a family history of Hodgkin lymphoma or CLL are at increased risk of developing these cancers themselves. Certain viral infections may also increase the risk of lymphomas. These include the Epstein-Barr virus, or EBV, the virus that causes infectious mononucleosis or mono; the human immunodeficiency virus, or HIV; and Kaposi sarcoma human immunodeficiency virus.
Pre-existing health conditions
Individuals with certain rare genetic conditions, including Down syndrome, Fanconi anemia, ataxia-telangiectasia, and Bloom syndrome, are at higher risk of developing leukemia.
The risk of blood cancers also may be increased in people who have abnormalities of the bone marrow such as myelodysplastic syndromes.
Symptoms
Symptoms of blood cancer can vary widely from person to person and over time, depending on the type and severity of the disease an individual has. Some blood cancers will grow for a long time before causing any noteworthy symptoms, while others may rapidly progress to cause symptoms.
Some common symptoms and signs of blood cancer are:
- fever or chills
- fatigue, weakness, or feeling foggy-headed or confused
- persistent or frequent headaches
- nausea, constipation, and/or loss of appetite
- a low white blood cell count, leading to frequent or unusually severe infections
- a low red blood cell count, leading to anemia
- sweating a lot, particularly at night
- shortness of breath
- unusually pale skin
- itchy skin or rash
- unexplained weight loss
- easy bruising or atypical bleeding, such as recurrent nosebleeds
- pain in the chest, abdomen, and/or bones
- swollen lymph nodes, which are usually most noticeable as lumps in the neck, underarm, and groin
- swelling of the liver and/or spleen, which commonly manifests as pain or discomfort in the belly.
These symptoms can occur in most types of blood cancer. A common symptom of myeloma that’s not typically seen in other blood cancers is feeling very thirsty and urinating more.
In addition to these disease signs, blood cancer symptoms in women may include vaginal bleeding or unusually heavy menstrual periods.
Many of the symptoms of blood cancer are nonspecific and are commonly seen in people who have other conditions. For example, swollen lymph nodes are common in children who have an infection, but can also be a sign of blood cancer in infants and children. When in doubt, one should talk to a doctor about any signs or symptoms that are causing concern.
Diagnosis
Diagnosing blood cancer usually starts with a medical examination in which a doctor will assess a patient’s symptoms and look for unusual bruising, swelling, and anything else that might be a sign of blood cancer.
If blood cancer is suspected, a range of blood cancer tests may be performed to further investigate. Because symptoms of blood cancer are often nonspecific and can overlap with other diseases, multiple tests often are needed to reach a correct diagnosis.
Getting an accurate diagnosis as early as possible is essential to facilitate prompt treatment and ensure the best possible clinical outcomes.
Blood cancer tests
There is no single blood test to detect cancer, but several different types of tests may be used to establish a blood cancer diagnosis:
- Blood tests may include a blood cell examination, in which an expert looks at blood cells under a microscope, blood cell counts that measure how many different types of cells are in the blood, or blood chemistry tests that look for unusual levels of other substances in the blood that may be a sign of cancer.
- Imaging tests, such as a CT scan, MRI, ultrasound, and/or X-ray, can be used to look for abnormal growths or bone damage that may be a sign of blood cancer.
- A bone marrow biopsy, in which a sample of cells from the bone marrow is collected to be analyzed in a laboratory, also can help to identify signs of these cancer types.
Treatment
There are a wide range of therapies available for blood cancer treatment. Patients should consult with their healthcare team to come up with a treatment plan that works for them. This entails discussing in detail the risks and benefits of each approach, and taking into account factors like the type of cancer and how fast it is progressing, the patient’s overall health and age, specific treatment side effects, and the patient’s wishes.
Treatment for blood cancers often involves combining multiple different approaches. There are many clinical studies continuously investigating new treatment options to improve patient care and survival rates.
Chemotherapy
Chemotherapy is a mainstay cancer treatment that uses chemicals that are toxic to rapidly growing cells, such as cancer cells. In addition to eliminating cancer cells, chemotherapy can also be used to help make other treatments more effective.
Dozens of different chemotherapy medications are approved and available; deciding which one(s) to use will depend on the particular type of cancer a patient has.
Chemotherapy can cause many side effects, including but not limited to:
- fatigue
- hair loss
- digestive upset
- difficulty concentrating
- pain
- mood changes.
Immunotherapy
Immunotherapies are medicines that unleash the immune system to attack cancer cells.
Different types of immunotherapies can either enhance the immune system’s ability to identify and combat cancer cells, or target specific proteins on cancer cells that normally allow them to evade the immune system.
Because this treatment approach works by activating the immune system, it often can cause side effects like:
- fever or flu-like symptoms
- fatigue
- nausea and vomiting
- diarrhea.
Radiotherapy
Radiotherapy uses radiation, or powerful beams of energy, that are directed toward areas where cancers are growing. It works to kill those cancer cells. Different types of radiotherapy may be used to treat blood cancer, depending on which parts of the patient’s body are affected.
While most blood cancers cannot be treated with radiotherapy alone, it’s often used in combination with other treatments, such as chemotherapy, or to relieve symptoms and improve quality of life.
Common side effects of radiotherapy include:
- fatigue
- hair loss
- nausea and vomiting
- reduced appetite
- skin problems.
Radiotherapy also may cause issues at the specific site being irradiated — for example, radiation near the mouth can cause dry mouth and difficulty swallowing.
Stem cell transplant
A stem cell transplant is a procedure that aims to replace the blood stem cells in a patient’s bone marrow with new, healthy ones. This can be curative for some types of blood cancer. However, the procedure is quite invasive, usually requiring weeks spent in the hospital, and high doses of chemotherapy before the transplant.
There are two types of stem cell transplants:
- autologous, which works by using a person’s own healthy stem cells to replace cells killed by cancer treatment
- allogeneic, whereby matching donor stem cells are used to replace unhealthy stem cells.
Stem cell transplants can carry risks such as:
- infections
- pain
- transplant rejection.
Surgery
Surgery may be used to remove a blood cancer if there is a clearly defined tumor that can be removed from the body. Surgery isn’t often used for blood cancers, but it may be an option in some types of lymphoma. Like any surgical procedure, blood cancer surgery carries risks, including bleeding and complications from anesthesia.
Other treatments
Blood cancer can also be treated using targeted therapy, a precise approach that zeros in on specific proteins, genes, or other parts of cancer cells that make them grow and spread.
By understanding the genetic or molecular changes in these cells, targeted therapy disrupts their growth signals while causing less harm to normal cells. This method often uses specialized drugs or antibodies that attach to particular targets on cancer cells.
In addition to treatments designed to address the cancer itself, people with blood cancer often benefit from other therapies that can help ease treatment side effects. Palliative care, which aims to manage pain and other symptoms, can help to improve patients’ quality of life.
Life expectancy and survival rate
Blood cancer can be life-threatening, but blood cancer prognosis has improved dramatically in recent decades thanks to modern medical treatments. In fact, for some types, the blood cancer survival rate has doubled or even quadrupled in recent years.
For leukemia, the overall five-year survival rate is 65%. In other words, about 2 of every 3 leukemia patients will still be alive five years after they are diagnosed. The prognosis varies substantially depending on the specific type of leukemia, however. For CLL, ALL, and CML, five-year survival rates are higher than 70%. For AML, they are slightly lower than 32%.
For Hodgkin lymphoma, the five-year survival rate is slightly less than 90%. In non-Hodgkin lymphoma, the overall five-year survival rate is 65%. In myeloma, the five-year survival rate is 58%.
Blood cancer life expectancy varies greatly depending on each individual’s situation. Among key factors are the specific type of cancer, how aggressive the cancer is and how far it’s spread, the patient’s age, and the existence of other co-occurring medical issues. Patients are advised to talk to their care team to understand the outlook for their specific situation.
Prevention and risk reduction
Because the causes of blood cancer aren’t fully understood, there is no definitive way to prevent blood cancer from developing. However, the chances of developing blood cancer can be minimized by taking steps to avoid risk factors such as:
- exposure to radiation
- chemicals
- cigarette smoke.
Maintaining healthy lifestyle habits, such as being physically active and eating a healthy diet, can also help mitigate risk factors associated with the development of blood cancer.
While it may not be possible to prevent blood cancer, early detection is crucial for people who have known risk factors. Being on the lookout for any potential signs of cancer and undergoing regular monitoring can help ensure that cancer can be identified and treated promptly if it develops.
Living with blood cancer
Maintaining good health is crucial for individuals living with blood cancer. While there isn’t a specific blood cancer diet, it’s generally recommended that individuals follow a balanced and nutritious eating plan. Because the disease and its treatments can affect appetite, it may be helpful for patients to consult with a nutritionist to ensure they’re getting all the nutrients they need.
Reducing the risk of infection is a critical aspect of managing blood cancer. Individuals living with blood cancer should practice good hygiene habits, such as washing their hands regularly and maintaining a clean environment. Additionally, limiting exposure to potential sources of infection, like avoiding close contact with sick individuals, is essential for maintaining overall health during treatment.
Fatigue is a common symptom experienced by those with blood cancer, both as a result of the disease itself and the treatments involved. It is essential for individuals undergoing blood cancer treatment to prioritize self-care and rest, taking time to recuperate.
Another crucial part of navigating life with blood cancer is looking out for one’s mental health. Mental health plays a vital role in the overall well-being of individuals living with blood cancer. The emotional challenges that accompany a cancer diagnosis can be overwhelming, and it’s essential for patients to seek support for their mental health needs.
Several resources are available, such as therapy and mindfulness programs, which can help patients navigate the emotional complexities of their journey.
Support groups also exist to help those affected by blood cancer. Among them are:
- the Leukemia and Lymphoma Society, which offers support groups and other resources for people with these forms of blood cancer
- the International Myeloma Foundation and Multiple Myeloma Research Foundation, both nonprofits offering support groups for people with myeloma.
Rare Cancer News can also be a resource for those with blood cancer, their caregivers, and their loved ones, providing the latest updates in research and treatment advances as well as educational resources.
Blood Cancer Awareness Month in September further unites the community, raising awareness and fostering support. Participation in this annual event sheds light on the challenges faced by those affected, while emphasizing the importance of continued research.
Rare Cancer News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Clearnote’s blood test uses AI to spot pancreatic cancer in high-risk groups
- Being a caregiver requires constant, sometimes impossible, calculations
- Immuno-gene therapy for brain cancer tumors now on FDA fast track
- FDA approves Keytruda for hard-to-treat gynecological cancers
- FDA reviewing new iberdomide combo for hard-to-treat multiple myeloma
Related article